Introduction
Intraoperative consultations in the form of frozen section play a vital role in the surgical management by avoiding extensive or second surgeries. The surgeon’s appropriate management and decision taking on the operating table depends on a frozen report that is as accurate as possible. Therefore it is critical to determine efficiency and audit the frozen section performance periodically. Audit also serves as an internal quality control, which will improve the quality of the service provided to the patient
Materials and Methods
This was a retrospective study undertaken at Saveetha medical college, Chennai. Complete enumerative sampling method was used. The records of 160 frozen sections and the corresponding final formalin fixed paraffin embedded (FFPE) histopathology reports during the study period of 2 years (2016–2018) were compared and analyzed.
In all the cases the frozen section analysis had been done on fresh tissue samples. After gross examination, the appropriate numbers of bits were taken depending on the nature of the tissue followed by snap freezing and sectioning of tissues using cryostat (Model: LEICA CM 1520). 4 microns thin sections were prepared, stained and re viewed bysenior experienced pathologist and the reports were conveyed to the operating surgeon. The time taken from receiving the specimen to conveying the diagnosis to the surgeon was noted in all cases. The remaining gross specimen and the frozen bits were fixed overnight in 10% neutral buffered formalin and processed routinely. The routine histopathology slides were reviewed by senior experienced pathologists and the final report was given.
The reports of the frozen section and FFPE tissue sections were compared and the results were categorized into concordant, discordant. The slides of the discordant cases were reviewed and the causes of discrepancy werenoted. The diagnostic accuracy and diagnostic error rates were calculated.
Results
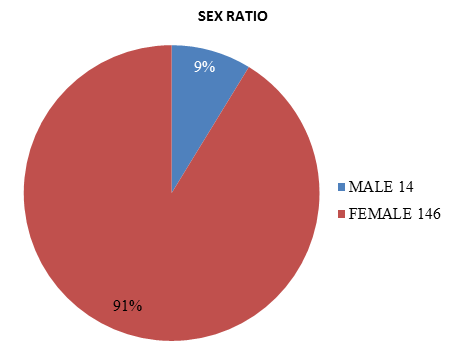
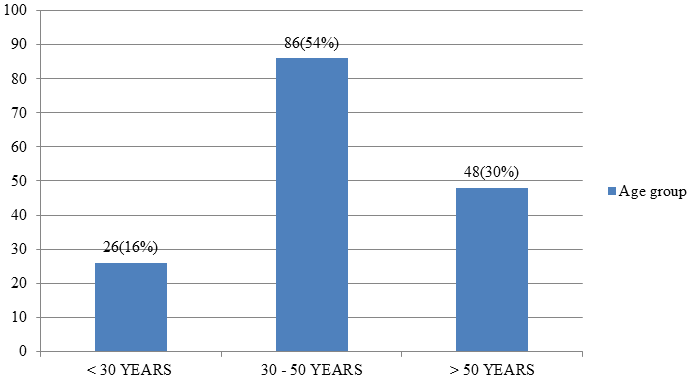
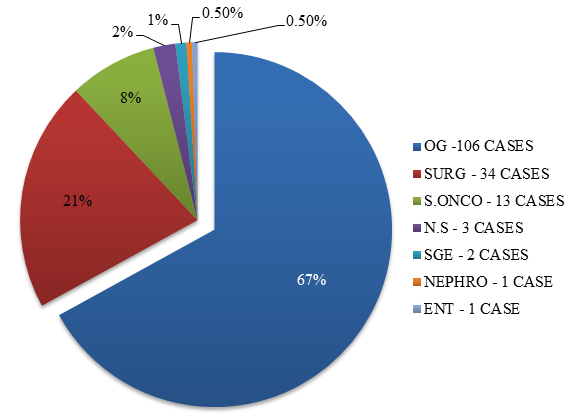
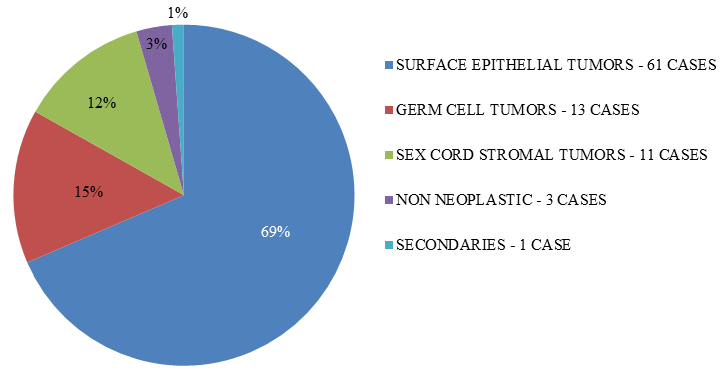
Out of 160 cases analyzed 146(91%) were from female patients and 14(9%) were from male patients (Figure 1). The most frequent age group in which frozen section consultation was sought was 30 – 50 years in 86 cases (54%) (Figure 2). Most number of frozen section consultations were from the department of Obstetrics and gynecology (106 cases, 67%), followed by the department of surgery (34 cases, 21%) and the department of surgical oncology (13 cases, 8%) (Figure 3). Ovary was the most frequent organ/ site sampled (89 cases) followed by the uterus (27 cases), thyroid (12 cases) and soft tissues (4 cases) (Table 1). Among the ovarian lesions surface epithelial tumors (69%) were the most common lesions sent followed by germ cell tumors (15%), sex cord stromal tumors (12%), non-neoplastic lesions (3%) and metastatic deposits (1%) (Figure 4). Average turnaround time for intra operative frozen section consultation in our study was around 15 minutes. 154 cases were concordant with the final histopathological diagnosis and 6 cases were discordant, which gives a discordance rate of 4% (Table 2). Among the discordant cases 5 were from the ovary and 1 was from soft tissue. The discordant cases are summarized in Table 3.
Discussion
Frozen section consults have become an important intra operative tool for making vital decisions like differentiating benign from malignant lesions or assessing surgical margins. Interpretation of intraoperative frozen section analysis requires sound theoretical knowledge, experience, basic understanding of clinical medicine, good judgment, capacity to make decisions under pressure and awareness of the limitations of this vital diagnostic procedure. The common indications for this procedure include confirmation/ruling out malignancy, determination of lymph node status, assessment of margins and assessment of adequacy of tissue (in poorly delineated lesions to avoid second biopsy). Discordance in the frozen section diagnosis and the final formalin fixed paraffin embedded tissue diagnosis can be due to 1. Technical issues (such as cutting, mounting, staining, mechanical issues in the cryostat etc.), 2. Limited sampling during frozen section analysis (as this procedure is time bound), 3. Interpretation or diagnostic errors, 4. Errors in communication of diagnosis etc. Therefore it is essential for all the centers practicing frozen section analysis to audit their frozen section consultations efficacy and performance periodically. The reason for discordance should be analyzed and care should be taken to avoid these errors in the future.
CAP standard for frozen section states that the turnaround time should be within 20 minutes,1,2 in our study we had an average turnaround time of 15 minutes. We also noted a significant female predilection (91%) this can be attributed to the importance of frozen section in gynec surgery as a majority of the cases we received for frozen section consultation were from the department of Obstetrics and gynecology.
In our study there were 6 discordant cases.
Table 1
Site/organ sampled for frozen section
Table 2
| Total No. of Cases | 160 |
| No of discordant cases | 6 |
| % Of concordant cases | 96% |
| % Of discordant cases | 4% |
Discordance rates
Table 3
Comparison of discordance rates with other studies
Table 4
Discordant cases
Figure 5
[ Case 1 ] A – Frozen section, H&E, 40x: ovarian cyst wall lined by mucin ous epithelium – Mucinous cystadenoma.. B – FFPE section, H&E, 40x : Foci of squamous epithelium – Benign cystic teratoma. [Case 2] C - Frozen section, H&E, 10x : F eatures of borderline mucinous tumor. D - FFPE section H&E, 10x : Evidence of invasion was noted – Mucinous carcinoma. [Case 3] E - Frozen section, H&E, 1 0x : Shows predominant areas of congestion and hemorrhage – Serous cystadenofibroma. F - FFPE section H&E, 10x : Tiny viable area showing features of borderline serous tumor.
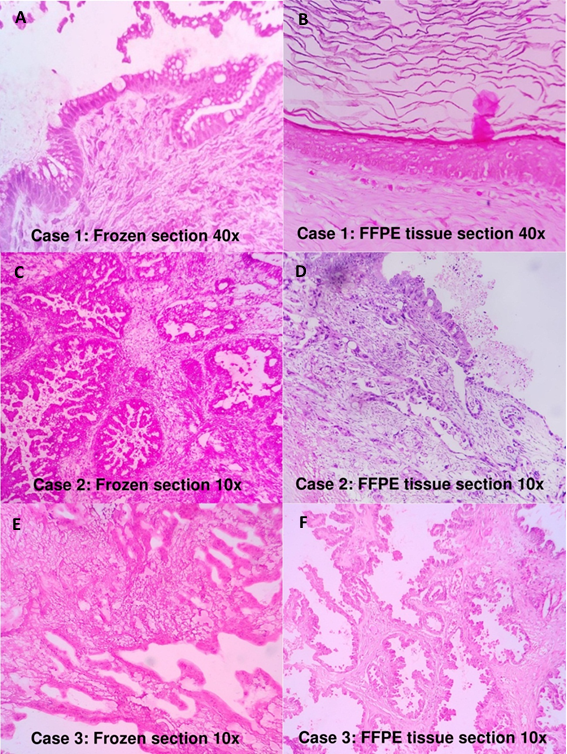
Figure 6
[Case 4] A – Frozen section, H&E, 10x Cyst wall lined by cuboidal to columnar cells with areas of stratification and mild atypia – Borderline serous tumor. B – FFPE section, H&E, 1 0x: fibrous cyst wall lined by cuboidal to low columnar ciliated epithelium - Serous cystadenofibroma. [Case 5] C - Frozen section, H&E, 10x : sheets and cords of neoplastic cells with abundant eosinophilic cytoplasm and pale nuclei resembling leydig cells – sertoli-leydig cell tumor. D - FFPE section H&E, 10x : Features of high grade serous carcinoma. [Case6] E - Frozen section, H&E, 40x : fascicles and interlacing bundles of spindle cells with mild nucleomegaly and no evidence of mitosis, pleomorphism and necrosis – Benign spindle cell lesion. F - FFPE section H&E, 40x : Mitosis and nuclear pleomorphism is evident – Malignant spindle cell lesion.

Case 1
Reported as mucinous cystadenoma in frozen section but turned out to be a benign cystic teratoma in final FFPE tissue report. The reason for this discordance was due to limited sampling of the gross specimen during frozen section analysis. Upon extensive sampling in formalin fixed tissue there were focal areas of neural tissue, squamous epithelium and smooth muscle bundles which prompted us to change the diagnosis.
Case 2
Reported asborderline mucinous tumor in frozen section but was signed out to be a mucinous carcinoma in final FFPE tissue report. This discordance was also due to limited sampling in frozen sections. Subsequent extensive sampling in formalin fixed tissue revealed areas of invasion.
Case 3
Reported as serous cystadenofibroma in frozen section but turned out to be a borderline serous tumor in final FFPE tissue report. Grossly the specimen of ovary received for frozen section analysis underwent torsion and was hemorrhagic, Microscopy showed predominant areas of congestion and hemorrhage, and one area showed cyst lined by single layer of cuboidal epithelium. Upon extensive sampling in formalin fixed tissue there was a tiny viable area showing features of borderline serous tumor.
Case 4
Reported as serous borderline tumor in frozen section but turned out to be a serous cystadenofibroma in final FFPE tissue report. Discordance was probably because the frozen section diagnosis was based on the gross findings such as numerous papillary excrescences which were reminiscent of borderline serous tumor; microscopy showed areas of stratification with mild atypia. Moreover CA 125 was mildly elevated. Tangential sectioning artifact of the frozen sections caused pseudo stratification of cells. Ice crystal artifacts and poor morphology of the cells also contributed to the discordance.
Case 5
Reported as sertoli-leydig cell tumor in frozen section but turned out to be a high grade serous carcinoma in final FFPE tissue report. Frozen section slides showed sheets and cords of neoplastic cells with abundant eosinophilic cytoplasm and pale nuclei resembling leydig cells. Clinically too, the patient had some features of virilisation. All these finding prompted the diagnosis of sertoli-leydig cell tumor. Discordance was due to poor morphology of the cells in frozen sections which led to an interpretation error.
Case 6
Reported as Benign spindle cell lesion in frozen section but turned out to be a malignant spindle cell tumor in the final FFPE tissue report. Features which are vital to make a diagnosis of malignant spindle cell lesion such as mitosis, nuclear pleomorphism, and necrosis were not appreciated in the frozen sections. Here too, the discordance was due to poor morphology in frozen sections which led to an interpretation error.
In our study discordance was primarily due to interpretation errors and errors due to limited sampling during frozen section. Interpretation error was also attributed to sectioning artifacts (freezing and folding), lack/poor quality of morphological details and presence of the diagnostic features in only in the deeper sections. The accuracy rate of frozen section analysis reported in the literature ranges from 92% to 97.98 %.5,8,9 Our study had an accuracy rate of 96% which was comparable with other studies.4,5,6,10