- Visibility 39 Views
- Downloads 8 Downloads
- DOI 10.18231/j.jdpo.2024.053
-
CrossMark
- Citation
Background
Mesenchymal tumors constitute only 5% of penile tumors, making them extremely uncommon. [1] Schwannomas, also known as, neurilemmomas are a class of nerve sheath tumors, made up of differentiated neoplastic Schwann cells. They are split into two distinct entities based on genetics, morphology, and clinical presentation. Conventional schwannoma, which is more frequently seen and benign, seldom develops malignant alterations. Melanotic schwannoma, on the other hand, is rare and has a low potential for malignancy. [2] Schwannomas have a low annual incidence of 0.6 per 100,000 people.[3] The most common sites are head and neck and extremities. It accounts for less than 1% of all penile tumors, making it a challenging clinical entity. The tumors are sporadic but maybe associated with genetic syndrome, neurofibromatosis. The majority of benign and malignant penile mesenchymal tumors present as asymptomatic, non-tender masses. We present a young male with mass on right penile shaft which was resected and histologically diagnosed as schwannoma. There is no recurrence on a follow-up of 6 months.
Case Presentation
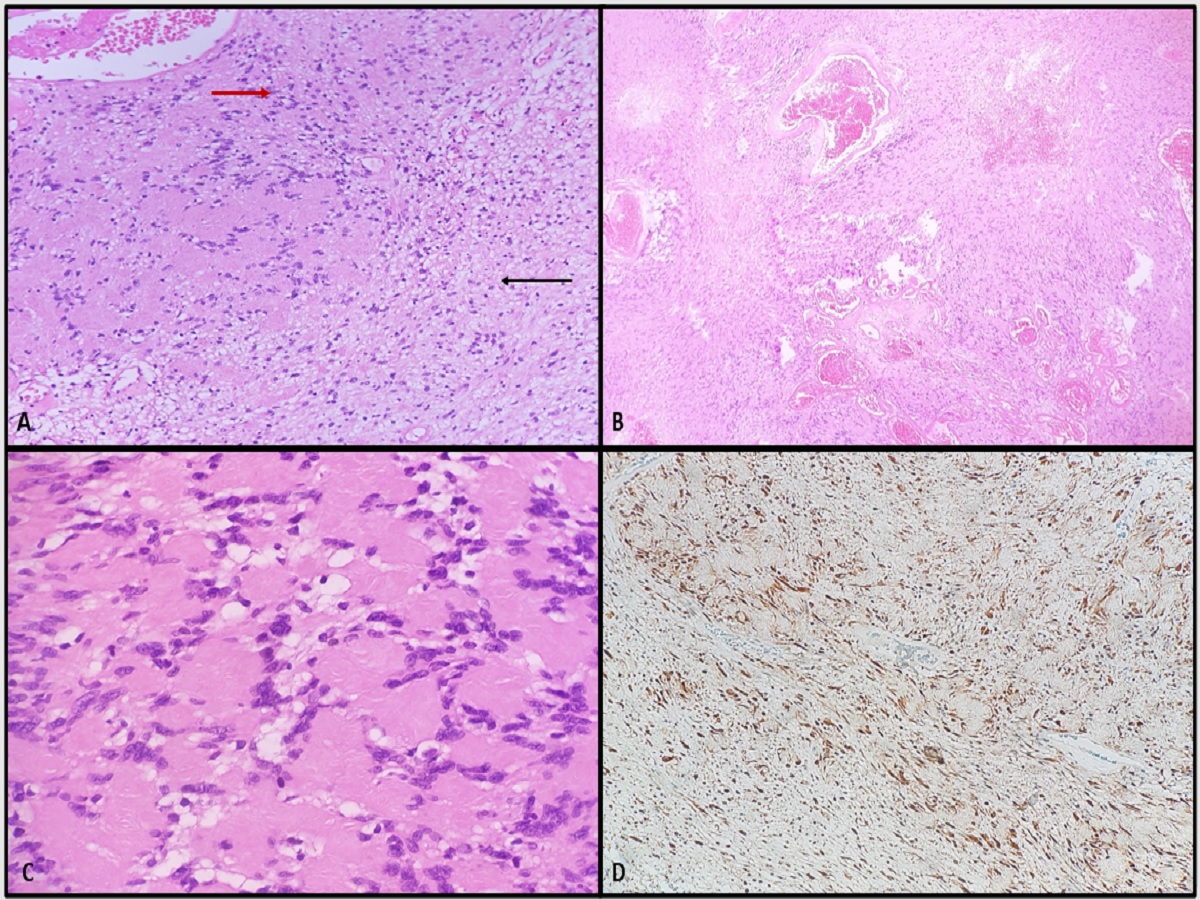
A 25-year-old man presented to urology department for evaluation of an asymptomatic mass on the right aspect of the penile shaft with distortion of penile curvature since childhood. On Magnetic resonance imaging (MRI) a well-defined lobulated soft tissue lesion at the right side of penile body measuring 2.3 x 2.7 x 4.4 cm was seen. The lesion shows central high T2 signal intensity with internal low T2 signal intensity focus likely calcification, peripheral intermediate, T2 signal intensity and diffusion restriction. In the postcontrast images, the lesion shows peripheral nodular discontinuous progressive enhancement. The lesion is abutting the right corpus cavernosum with no gross invasion. The corpus spongiosum and left corpus cavernosum, both testis and spermatic cords, visualized part of pelvic organs were unremarkable. No pelvic free fluid, collection or significant lymph nodes were noted. The imaged soft tissue and osseous structures were unremarkable ([Figure 1] ). It was suggestive of a benign vascular penile lesion; differential diagnosis included hemangioma or neoplastic lesion. On resection the mass was encapsulated and circumscribed, not involving the deep layers of the penis. During microscopic examination, hematoxylin-eosin staining revealed cellular spindle cells arranged in a palisading fashion(Verocay bodies). At places, the tumor cells were separated by edematous fluid. Thick-walled hyalinized blood vessels were seen with rare mitosis([Figure 2] A-C). Immunohistochemistry for S-100 immunoperoxidase was positive([Figure 2] D) and negative for desmin. A diagnosis of schwannoma was made and no recurrence has been observed after 6 months follow-up period.

Discussion
Schwannomas are benign tumors of the peripheral nerve sheath made up of Schwann cells. The incidence of peripheral schwannomas was reported to be 0.6 per 100,000 people. [3] The highest incidence occurs during the fourth and sixth decades of life, with no gender preference. Peripheral nerves in the skin and subcutaneous tissue of the head and neck, as well as along the flexor surfaces of the extremities [2] are the most common sites of origin. The vast majority of cases are sporadic, with only a small percentage associated with type 2 neurofibromatosis, caused by a germline mutation in the NF2 gene on 22q12, which produces merlin, also known as schwannomin. [4] Schwannomas of the penis are extremely uncommon, with the first case reported in 1968. [3] In English literature, Dehner and Smith reported the first three cases of penile schwannomas in 1970. [5]
The most common site of penile schwannomas is the penile shaft, predominant presentation as a solitary mass. [6] They are slow-growing tumors that frequently present as asymptomatic nodules or as incidental findings on imaging investigations. Pain can be felt if the lesion grows between the Buck fascia and the tunica albuginea, according to Lee et al.[7] Sexual dysfunction such as erectile dysfunction, aberrant penile curvature, pain with ejaculation, Peyronie's disease, impotence, and pain with intercourse can be associated findings.[8] Dyspareunia was found to be the commonest symptom for sexual dysfunction. [9]
Radiologically, ultrasonography(USG) is less helpful in diagnosing penile schwannomas than magnetic resonance imaging(MRI), which can aid in preoperative diagnosis.[7] Schwannomas are typically well-defined, hypervascular on color Doppler USG, and hypoechoic on gray-scale USG. Their low to moderate signal intensity on T1-weighted images and their inhomogeneous high signal intensity on T2-weighted images have been demonstrated by MRI. Masses that are homogenously enhanced, low density, and clearly margined have been discovered using computed tomography. [10]
Histopathologically, the tumor has a unique microscopic appearance with Antoni A and B areas. The Antoni A zones are mostly made up of spindle cells that are frequently grouped in an organoid or palisading pattern (Verocay bodies). There may be cystic areas that separate the tumor cells in Antoni B zones. Typically, thick-walled hyalinized blood vessels are present, sometimes with thrombosis. Prominent nuclear palisading is a characteristic that is not specific to schwannoma; smooth muscle tumors can also exhibit it in certain situations. S-100 protein, calretinin (as opposed to neurofibromas), and basal lamina constituents(such laminin and type IV collagen) are all immunoreactive in the tumor cells.[4] Differential diagnosis of this superficial tumor in the penis should include leiomyoma, sarcoma, Peyronie’s disease and fibrosis.
Surgical removal is the treatment of choice with complete excision of the mass, and care taken for the nerve supply. Recurrence of schwannoma is uncommon. Preserving sexual function is the main goal in the management of penile schwannoma.[11] The dorsal nerves are sensory nerves supplying the urethra, glans, and penile shaft. Planning the amount of the excision and maintaining tunica albuginea, which avoids penile curvature and erectile dysfunction, depend on the preoperative evaluation of the tumor. [8] Prioritizing lesions that cause symptoms while preserving the remaining lesions may maximize symptom reduction and reduce nerve damage. [12]
Conclusion
Schwannomas are uncommon mesenchymal tumors which are rarely encountered in penis. They usually present as slow growing, asymptomatic mass in dorsal penile shaft. MRI can point to diagnosis; however histopathology is confirmatory. Treatment is surgical excision with rare recurrence and excellent prognosis.
Source of Funding
None.
Conflict of Interest
None.
References
- M Miettinen, H Moch, PA Humphrey, TM Ulbright, VE Reuter. . World Health Organization Classification of Tumours of the Urinary System and Male Genital Organs 2016. [Google Scholar]
- CR Antonescu, A Perry, JM Woodruff, Schwannoma, CDM Fletcher, JA Bridge. . Mertens F, editors. World Health Organization Classification of Tumours of Soft Tissue and Bone 2013. [Google Scholar]
- CA Parra. Solitäres Neurinom der Glans penis. Dermatologica 1968. [Google Scholar]
- J R Goldbum. . Soft Tissue. Rosai and Ackerman’s Surgical Pathology 2017. [Google Scholar]
- LP Dehner, BH Smith. Soft tissue tumors of the penis. A clinicopathologic study of 46 cases. Cancer 1970. [Google Scholar]
- SH Kim, H Ahn, KH Kim, DS Kim, HJ Yang. Penile schwannoma mistaken for hemangioma: a rare case report and literature review. Transl Androl Urol 2021. [Google Scholar]
- CH Lee, CJ Wu, YL Chen, GS Huang, SH Tang. Case report on multiple penile schwannomas and their magnetic resonance imaging characteristics. J Androl 2012. [Google Scholar]
- AH Nguyen, ML Smith, EL Maranda, S Punnen. Clinical features and treatment of penile schwannoma: a systematic review. Clin Genitourin Cancer 2016. [Google Scholar]
- LC Huang, HZ Wang, YC Chu, KF Ng, CK Chuang. Clinicopathological presentation and management of penile schwannoma. Sex Med Rev 2020. [Google Scholar]
- DC Jung, SII Hwang, SII Jung, SH Kim, SH Kim. Neurilemmoma of the glans penis: ultrasonography and magnetic resonance imaging findings. J Comput Assist Tomogr 2006. [Google Scholar]
- R Jiang, JH Chen, M Chen, QM Li. Male genital schwannoma, review of 5 cases. Asian J Androl 2003. [Google Scholar]
- SS Voleti, CJ Warren, NR Parker, M Stanton, AA Khan, SS Noland. Excision of recurrent penile schwannoma with neurovascular bundle sparing: A novel surgical approach. Urol Case Rep. Urol Case Rep 2023. [Google Scholar]
