- Visibility 341 Views
- Downloads 61 Downloads
- Permissions
- DOI 10.18231/j.jdpo.2024.048
-
CrossMark
- Citation
Non-tumor associated Psammoma bodies in cervical lymph node: A case report
Abstract
Psammoma Bodies (PBs), associated with thyroid carcinomas, raise diagnostic challenges when found without concurrent papillary thyroid carcinoma (PTC). This report presents a case of PBs in cervical lymph nodes without evidence of thyroid malignancy.
A 53-year-old woman with neck swelling underwent total thyroidectomy. Despite PBs in cervical lymph nodes, microscopic examination revealed thyroid follicular nodular disease with no evidence of PTC.
This case questions the diagnostic reliability of PBs without PTC. The study by Hunt et al. emphasized the potential for PTC detection in cases initially labeled as PBs-only, stressing the need for comprehensive evaluation.
Differential diagnoses and the need for clinical correlation highlight the complexity of interpreting PBs without PTC. Seeking a second opinion and additional diagnostic tools may be crucial.
PBs, despite their strong link to PTC, may not conclusively indicate malignancy when found alone. Management decisions should consider clinical context, patient history, and available diagnostic tools. Further exploration of PBs in benign thyroid conditions is encouraged for improved understanding and diagnostic accuracy in larger series. Collaborative efforts between pathologists and clinicians are essential for optimal patient care in such challenging cases.
Introduction
Psammoma Bodies (PB), are characterised by round to oval calcifications with typical lamellation according to morphological features, and have sparked debates about their origin. Some propose that they signify a process of dystrophic calcification, often associated with the potential thrombosis in the papillary fibrovascular core or the necrotic evolution of a lymphatic metastasis.[1] PBs are most commonly observed in papillary thyroid carcinoma (PTC), meningioma, and papillary serous cystadenocarcinoma of the ovary. [2]
Implicit in these definitions is the strong association of PBs with thyroid carcinoma, particularly in the context of PTCs and some of its subtypes. However, the presence of PBs without evidence of PTC raises interpretative challenges. To date, the consensus among most authors is that although PBs may occur in a few benign conditions, they should be considered an extremely rare occurrence. [3]
Case Presentation
A 53 year old lady with no known comorbidities presented with neck swelling on April 2023. There was no recent increase in size. USG thyroid showed enlarged thyroid gland with multiple nodules (ACR TR 4, ACR TR 3) and retrosternal extension along with cervical lymphadenopathy on right side. Lower pole of left lobe of thyroid showed a solid nodule with echogenic foci measuring 0.9x0.7cms-(ACR TR5). CECT chest showed assymetric multinodular goitre with retrosternal extension, cervical and mediastinal lymphadenopathy. USG guided FNA was suggestive of benign follicular nodule –Bethesda category II.
Total thyroidectomy with bilateral neck node dissection was done after taking proper consent. Macroscopic evaluation revealed a 75 g thyroid with multiple colloid-filled nodules on both lobes and foci of calcification in the lower pole of the left lobe. No other whitish/ hard areas were identified. Thyroid was extensively sampled. 4 lymph nodes were isolated from right neck node dissection sample and 1 lymph node from left neck node dissection sample.
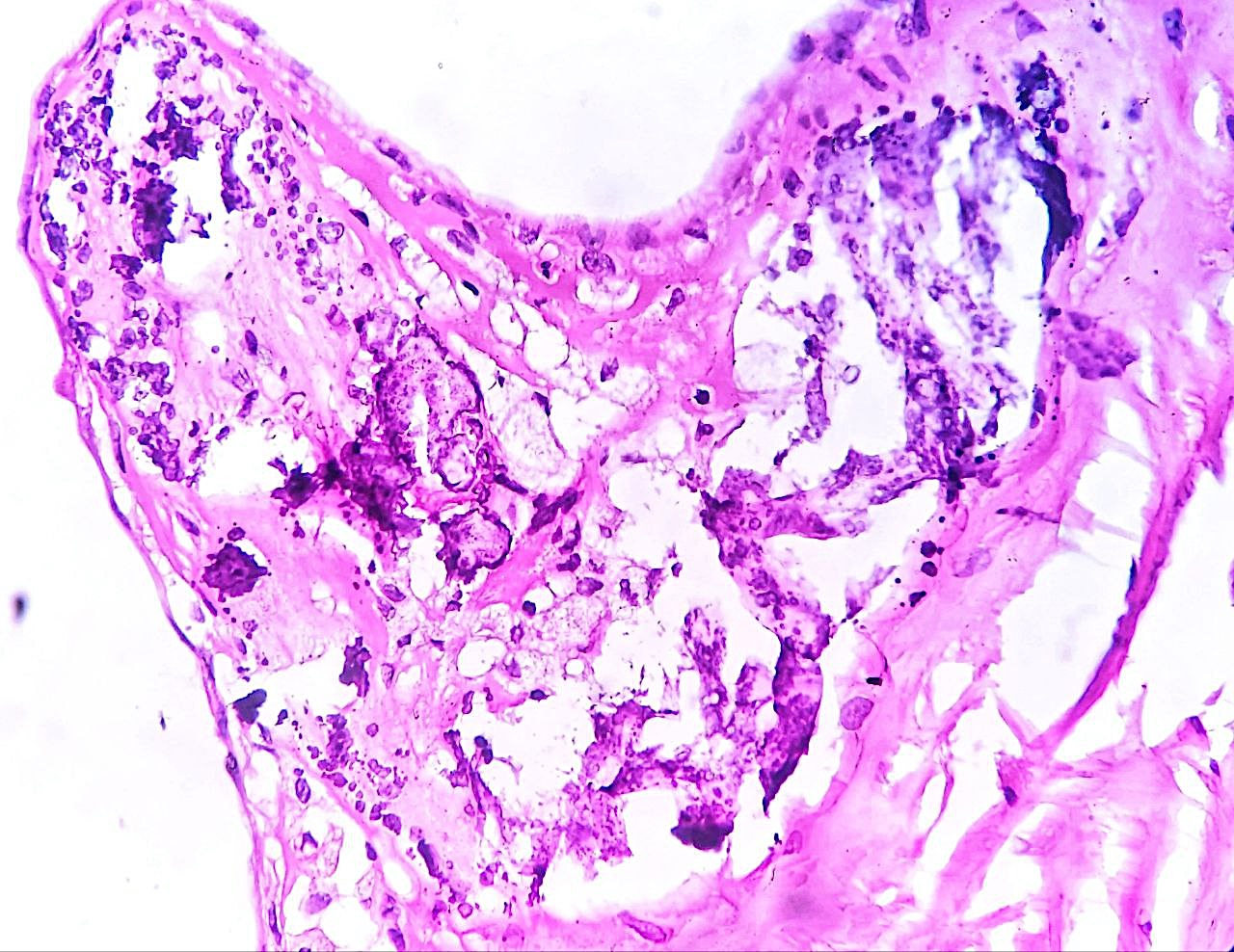
Microscopic examination revealed only thyroid follicular nodular disease with focal degenerative changes and calcifications.([Figure 1])
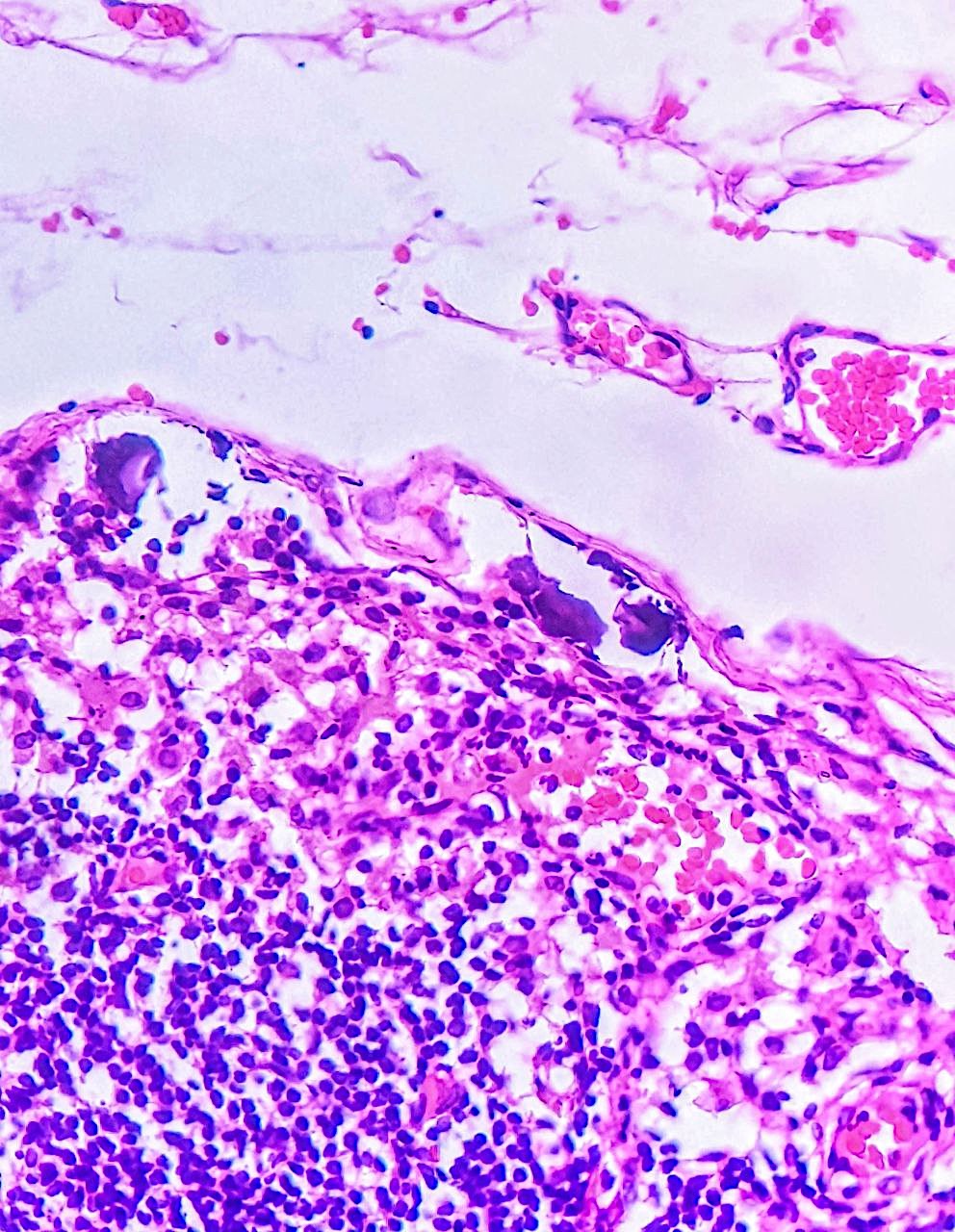
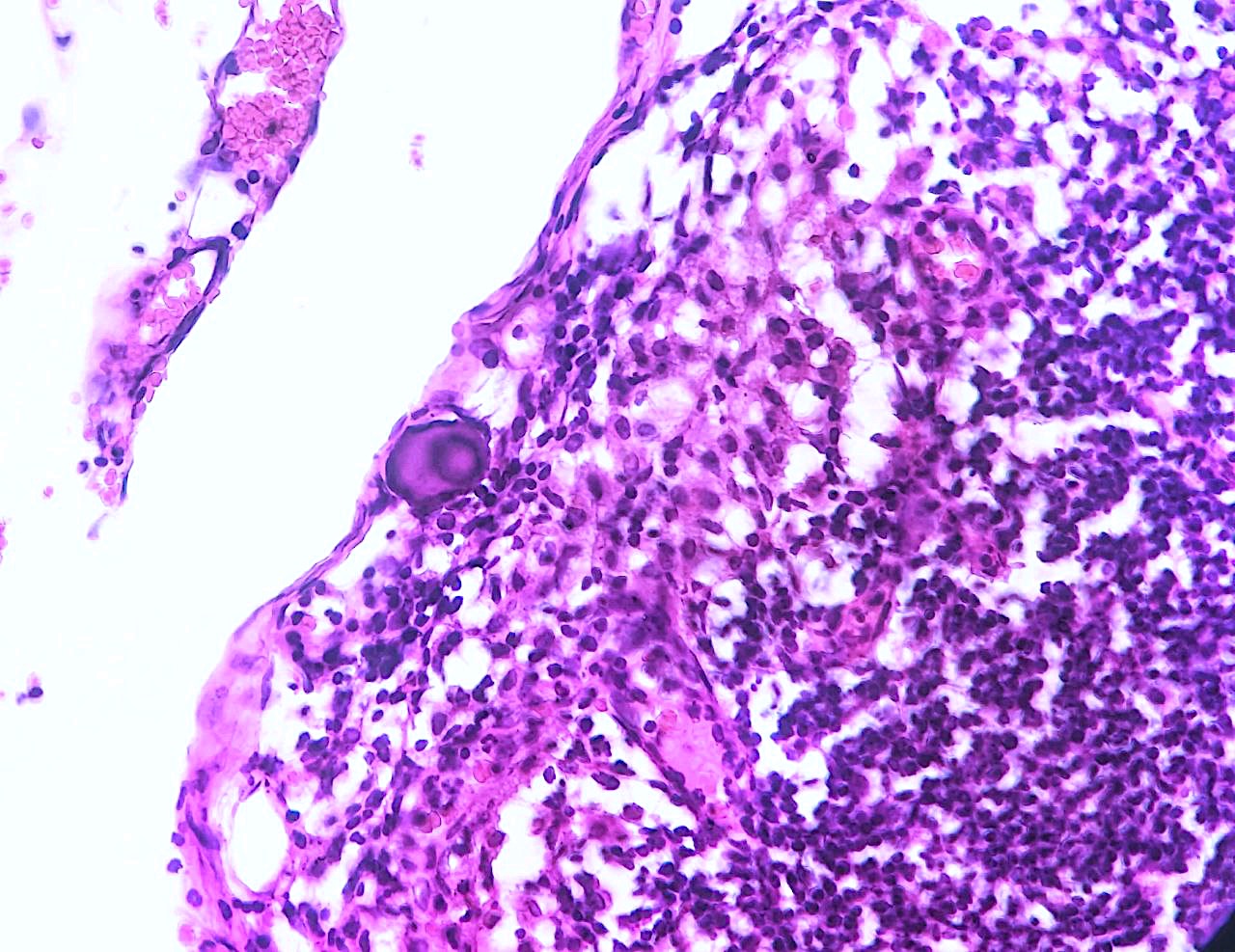
2/4 right cervical lymph nodes showed psammoma bodies in the subcapsular sinus.([Figure 2], [Figure 3]) Extensive sampling was conducted on both thyroid lobes to meticulously study the potential presence of papillary thyroid carcinoma (PTC). Multiple cut levels were examined in the thorough evaluation, yet no evidence of PTC was confirmed. The surgeons verified the complete removal of the entire thyroid tissue, with no macroscopic indications of residual thyroid tissue. Given the presence of several Psammoma Bodies (PBs), a note was added, highlighting the incidental detection of PBs and confirming the absence of any PTC. We recommended a rigorous clinical follow-up for the patient.
Discussion
In a paper by Hunt et al. the authors described the clinical, pathological and follow-up data of 29 patients with PBs, without the detection of thyroid carcinoma. [1] According to their results, in 27 of 29 cases there was a PTC after an accurate inclusion of all thyroid tissue, while the 2 remaining cases did not show evidence of malignancy. In their analysis, the authors emphasised that these two latter patients underwent only a lobectomy, so a complete inclusion and evaluation of all thyroid tissue had not been provided. [1]
In a review article, Ferreira et al. emphasized that the major highlight is based on the suggestion to discriminate PBs from other types of micro and macro-calcifications in the contest of thyroid lesions.[2] The pathognomonic characteristics of PB can be identified in the typical concentric lamellation and the lack of birefringence. The latter finding is absent in oxalate crystals and other calcifications in the contest of thyroid tissue. According to these morphological criteria, our case confirmed the morphological features of PBs. [2]
Locoregional recurrence is a significant problem for those with differentiated thyroid cancer with reported rates between 20% and 59% depending on tumour characteristics.[4], [5], [6] The link between the presence of lymph node metastatic disease and increased locoregional recurrence has been demonstrated by multiple authors. Reporting of “psammoma bodies only” in lymph nodes is not well defined. While indolent, they do indicate capacity for lymphatic spread and are considered pN1a in the presence of primary in thyroid. [7], [8], [9]
Spontaneous cancer regression is a rare phenomenon that has been reported in various types of cancers, including neuroblastoma, choriocarcinoma, malignant melanoma, lymphoma, renal cell carcinoma, and breast and colon cancer.[10], [11], [12] The mechanism of spontaneous regression is poorly understood, but some of the proposed mechanisms include immune mediation, growth factor and cytokine-mediated mechanism, and hormonal mediation.[13] Regression of papillary carcinoma thyroid has been reported. [14]
Despite the well-established association between PBs and thyroid carcinomas, and significance of their presence in lymph nodes, the detection of only PBs can often present a diagnostic dilemma.
In this specific case, we conducted a comprehensive examination of the entire thyroid tissue at multiple levels. Despite a thorough analysis, we found no evidence of classic papillary thyroid carcinoma (PTC) or any of its subtypes. The meticulous search for carcinoma foci yielded consistently negative results.
There are several considerations and potential scenarios in such cases:
Benign Conditions: PBs can also be seen in benign conditions such as nodular hyperplasia, adenomas, or other non-malignant thyroid lesions. Therefore, the presence of PBs alone may not always indicate malignancy.
Occult or Microscopic Lesions: In some cases, primary thyroid carcinoma may be microscopic or occult, not detectable by routine histological examination. Additional techniques like immunohistochemistry or molecular studies may be required to identify subtle malignant changes.
Differential Diagnosis: The absence of classic PTC features on routine examination suggests the need to consider other differential diagnoses, such as follicular adenomas or other rare thyroid neoplasms.
Clinical Correlation: Clinical information, including patient history, imaging studies, and other diagnostic tests, can provide an important context for the interpretation of histological findings.
Second Opinion: Given the complexity of thyroid pathology, seeking a second opinion from experienced pathologists or consulting a multidisciplinary team can be valuable in challenging cases.
Conclusion
The presence of PBs in thyroid tissue without the detection of classic papillary thyroid carcinoma (PTC) or any subtype of PTC can indeed pose a diagnostic challenge. Although PBs are strongly associated with thyroid carcinomas, especially PTC, their presence alone may not be sufficient for a definitive diagnosis of malignancy.
Regarding the management of cases where PBs are found in a lobectomy without evidence of classic PTC, decisions will depend on various factors, including the overall clinical context, the patient's history, and the available diagnostic tools. It may involve close clinical follow-up, additional imaging studies, or even consideration of further surgical procedures if warranted.
In conclusion, while PBs are strongly associated with PTC, their presence alone may not provide a definitive diagnosis of malignancy. Interpreting such cases requires careful consideration of various factors, and collaboration between pathologists and clinicians is crucial for optimal patient management. The authors hope that others will share their experience with the detection of PBs in benign thyroid conditions, so that the finding could be studied and confirmed in larger series as a possible diagnostic finding.
Source of Funding
None.
Conflict of Interest
None.
References
- Cardisciani L, Policardo F, Tralongo P, Fiorentino V, Rossi E. What psammoma bodies can represent in the thyroid: what we recently learnt from a story of lack of evidence. Pathologica. 2022;114(5):373-5. [Google Scholar]
- Ferreira L, Gimba E, Vinagre J, MS, Soares P. Molecular aspects of thyroid calcification. Int J Mol Sci. 2020;21(20). [Google Scholar]
- Hunt J, Barnes E. Non-tumor-associated psammoma bodies in the thyroid. Am J Clin Pathol. 2003;119(1):90-4. [Google Scholar]
- Mcconahey W, Hay I, Woolner L, Heerden J, Taylor W. Papillary thyroid cancer treated at the Mayo Clinic, 1946 through 1970: initial manifestations, pathologic findings, therapy, and outcome. Mayo Clin Proc. 1986;61(12):978-96. [Google Scholar]
- Byar D, Green S, Dor P, Williams E, Colon J, Gilse H. A prognostic index for thyroid carcinoma: a study of the E.O.R.T.C. thyroid cancer cooperative group. Eur J Cancer. 1979;15(8):1033-41. [Google Scholar]
- Mazzaferri E, Young R. Papillary thyroid carcinoma: a 10-year follow-up report of the impact of therapy in 576 patients. Am J Med. 1981;70(3):511-8. [Google Scholar]
- Cranshaw I, Carnaille B. Micrometastases in thyroid cancer: an important finding?. Surg Oncol. 2008;17(3):253-8. [Google Scholar]
- Urken M, Mechanick J, Sarlin J, Scherl S, Wenig B. Pathologic reporting of lymph node metastases in differentiated thyroid cancer: a call to action for the College of American Pathologists. Endocr Pathol. 2014;25(3):214-8. [Google Scholar]
- Randolph G, Duh Q, Heller K. The prognostic significance of nodal metastases from papillary thyroid carcinoma can be stratified based on the size and number of metastatic lymph nodes, as well as the presence of extranodal extension. Thyroid. 2012;22(11):1144-52. [Google Scholar]
- Everson T. Spontaneous regression of cancer. Ann NY Acad Sci. 1964;114(2):721-35. [Google Scholar]
- Sasaki J, Kurihara H, Nakano Y, Kotani K, Tame E, Sasaki A. Apparent spontaneous regression of malignant neoplasms after radiography: report of four cases. Int J Surg Case Rep. 2016;25:40-3. [Google Scholar]
- Chida K, Nakanishi K, Shomura H, Homma S. Spontaneous regression of transverse colon cancer: a case report. Surg Case Rep. 2017;3. [Google Scholar]
- Papac R. Spontaneous regression of cancer: possible mechanisms. In Vivo. In Vivo. 1998;12(6):571-8. [Google Scholar]
- Shim J, Rao J, Yu R. Spontaneous regression of metastatic papillary thyroid cancer in a lymph node: case report and literature review. Case Rep Endocrinol. Case Rep Endocrinol. 2018. [Google Scholar] [Crossref]
How to Cite This Article
Vancouver
James N, Thomas M, Pothen L, Thomas SM, Mathews R. Non-tumor associated Psammoma bodies in cervical lymph node: A case report [Internet]. IP J Diagn Pathol Oncol. 2024 [cited 2025 Sep 29];9(4):234-237. Available from: https://doi.org/10.18231/j.jdpo.2024.048
APA
James, N., Thomas, M., Pothen, L., Thomas, S. M., Mathews, R. (2024). Non-tumor associated Psammoma bodies in cervical lymph node: A case report. IP J Diagn Pathol Oncol, 9(4), 234-237. https://doi.org/10.18231/j.jdpo.2024.048
MLA
James, Nikita, Thomas, Meeta, Pothen, Lillykutty, Thomas, Sonia Mary, Mathews, Rebecca. "Non-tumor associated Psammoma bodies in cervical lymph node: A case report." IP J Diagn Pathol Oncol, vol. 9, no. 4, 2024, pp. 234-237. https://doi.org/10.18231/j.jdpo.2024.048
Chicago
James, N., Thomas, M., Pothen, L., Thomas, S. M., Mathews, R.. "Non-tumor associated Psammoma bodies in cervical lymph node: A case report." IP J Diagn Pathol Oncol 9, no. 4 (2024): 234-237. https://doi.org/10.18231/j.jdpo.2024.048
