- Visibility 167 Views
- Downloads 16 Downloads
- DOI 10.18231/j.jdpo.2024.047
-
CrossMark
- Citation
Atypical stromal cells, a pseudosarcomatous change in sinonasal polyp causing diagnostic dilemma - A case report and review of literature
Introduction
Nasal polyposis is a commonly encountered non-neoplastic inflammatory disease of the nose and paranasal sinuses presenting with various clinical manifestations like nasal obstruction, rhinorrhea, headache, anosmia/hyposmia, etc.[1], [2] The incidence of nasal polyposis in the general population is 0.5 to 4%.[2] The two most common etiologies of nasal polyps includes allergy and infections.[3] The histological diagnosis of benign inflammatory polyps of the nasal cavity usually doesnot pose any diagnostic difficulties. Certain unusual histological features like presence of amyloid, atypical stromal cells can be rarely observed in a nasal polyp which might be a huge challenge to the pathologists as they mimic sarcoma. [4], [5] We hereby present one of the unusual feature – atypical stromal cells in a nasal polyp which we came across during histopathological examination of an antrochonal polyp from a 34 year old female who presented with bilateral nasal obstruction. Pathologists and clinicians must be well aware of this entity, though they are rare. A better understanding of this entity – presence of atypical stromal cells in a benign inflammatory polyp can help in preventing an erroneous diagnosis of sarcoma, thereby preventing unnecessary treatment and anxiety to the patient.
Case Presentation
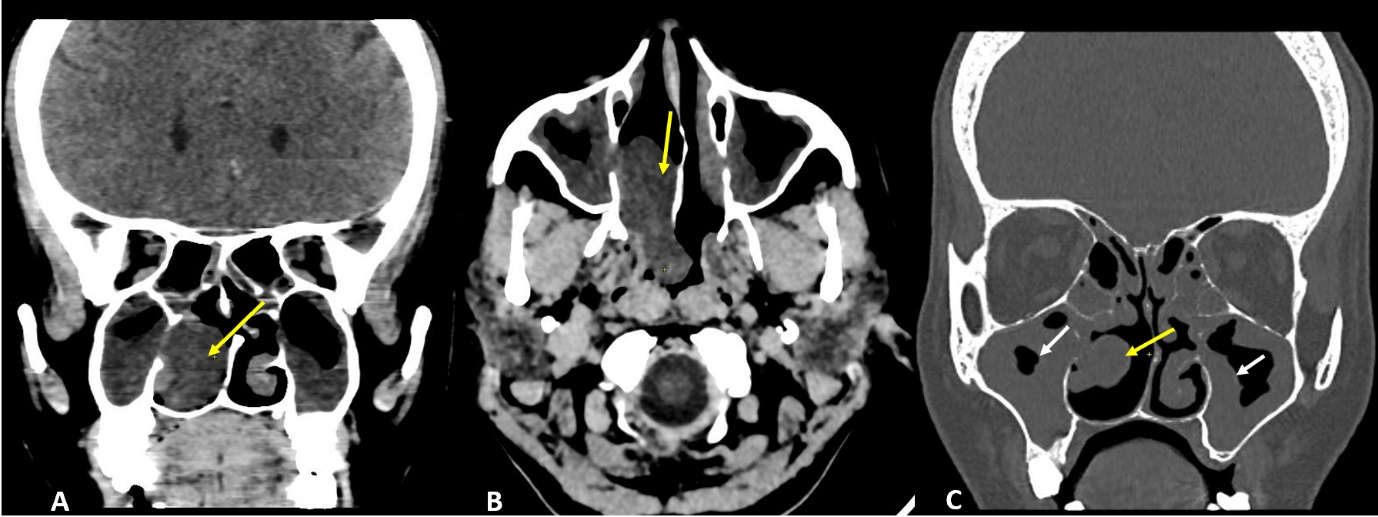
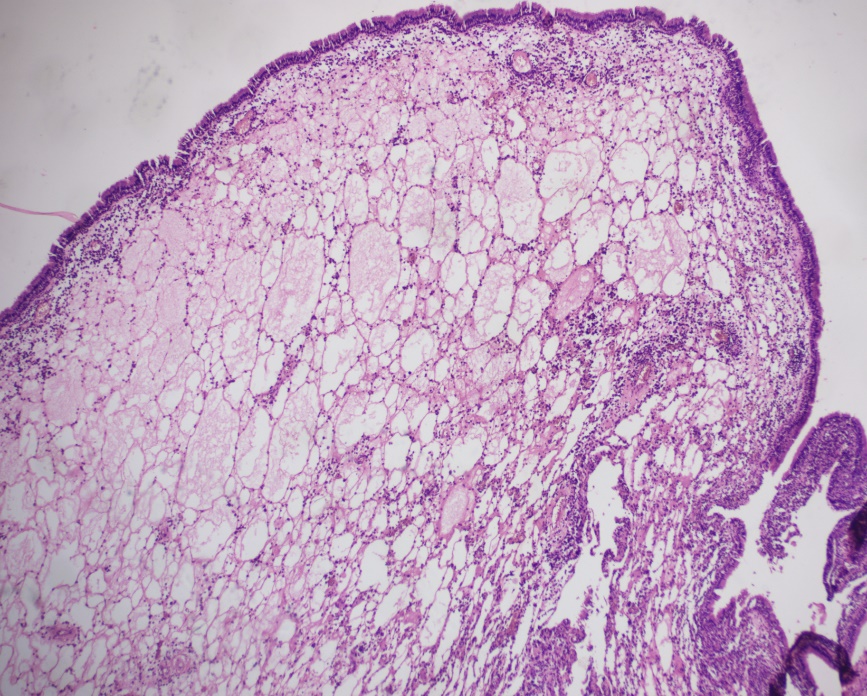
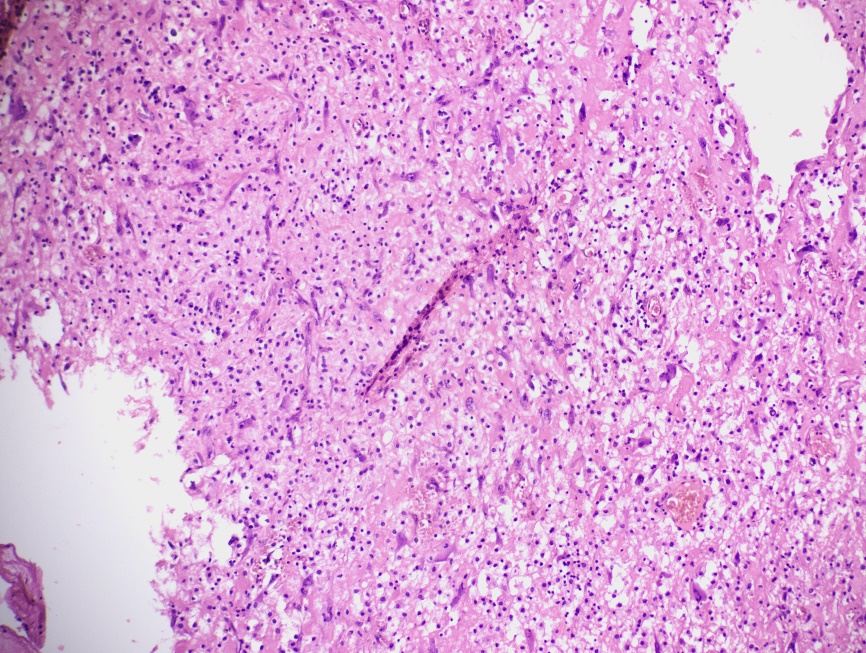
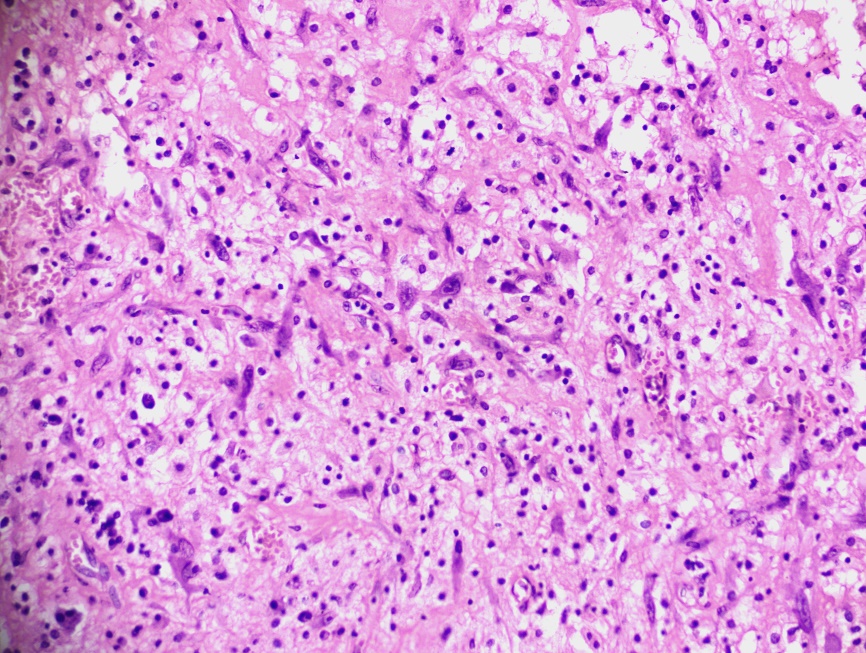
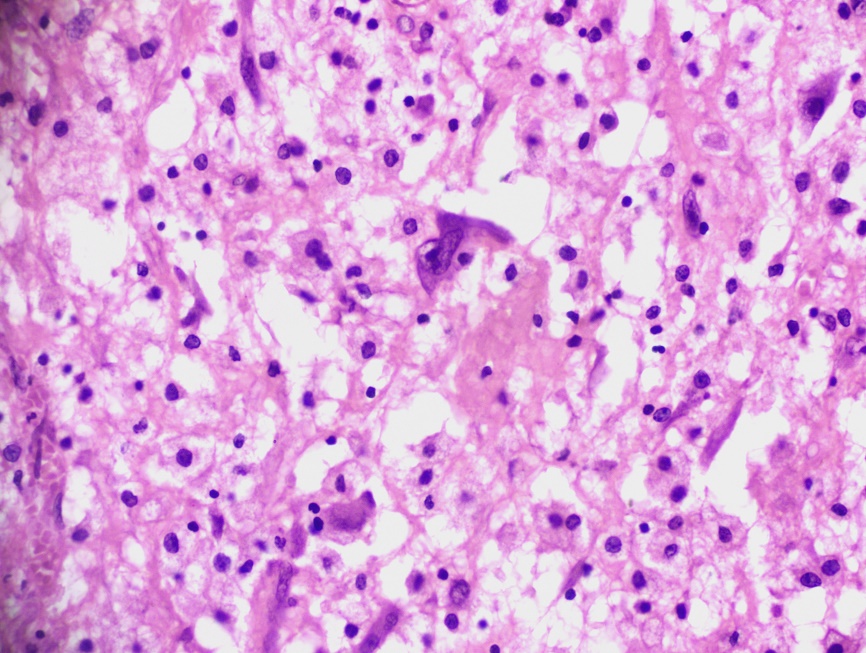
A 34 year old female presented with bilateral nasal obstruction since 7 months, history of nasal discharge and hyposmia. On anterior rhinoscopic examination, there was a smooth greyish white solitary polypoidal mass along with mucoid discharge seen in right nasal cavity and subsequent nasal endoscopic examination revealed presence of a polypoidal mass occupying posterior part of nasal cavity going into nasopharynx and on probing the mass was seen to arise from sphenoethmoidal recess and was not sensitive or does not bleed on touch and hence diagnosis of right sphenochoanal polyp was made. A diagnosis of deviated nasal septum with chronic rhinosinusitis and right antrochoanal polyp was made and the patient was posted for Septoplasty with FESS under General anaesthesia CT Paranasal sinuses (with contrast) showed a well-defined non enhancing polypoidal lesion in the right nasal cavity in the middle meatus extending to the nasopharynx posteriorly. Lesion was abutting the maxillary infundibulum and the inferior turbinate, causing obstruction of the osteomeatal unit. Imaging findings were suggestive of benign – possibly inflammatory nasal polyp. Polypoidal mucosal thickening also noted in the bilateral maxillary and the sphenoid sinuses ([Figure 1] ). Intraoperative findings were deviated nasal septum to left. Smooth ulcerated mass/polyp seen arising from right sphenoidal ostia, polypoid change noted in bilateral maxillary, ethmoidal and sphenoidal sinuses. Histopathological examination showed an inflammatory polyp with focal squamous metaplasia, ulceration, areas of acute suppurative inflammation, atypical stromal cells and calcification([Figure 2], [Figure 3], [Figure 4], [Figure 5]). Few blood vessels with intraluminal thrombi were also noted. There were no granuloma, allergic mucin, fungal organisms or any evidence of dysplasia or malignancy in the sections examined.
Discussion
Nasal polyposis - benign inflammatory hyperplastic outgrowths of the sinonasal mucosa is a commonly encountered non-neoplastic inflammatory disease of the nose and paranasal sinuses presenting with various clinical manifestations like nasal obstruction, rhinorrhoea, headache, anosmia/hyposmia, etc. Nasal polyps(NPs) were known at the time of the Egyptians. About 150 years ago, Hippocrates introduced the term “polyp” and described the first procedure for their removal. The incidence of nasal polyposis in the general population is 0.5 to 4%.[6] On gross examination, polyps are usually pale grey to pink soft glistening masses. Allergy and infection are the most important causes of nasal polyps. Nasal polyps are usually associated with chronic rhinosinusitis. Certain other causes of nasal polyposis includes cystic fibrosis. Any young patient with refractory nasal polyposis, possibility of cystic fibrosis needs exclusion. Nasal polyps are usually due to the result of T-helper 2 cell-driven eosinophilia, immunoglobulin-E (IgE) inflammation with elevated interleukin-5 (IL-5) together with environmental and/or seasonal allergic triggers. 25%-30% of patients with chronic rhinosinusitis have nasal polyps. Chronic rhinosinusitis with nasal polyps usually affects patients between 40 to 60 years of age. Males are more likely to be affected as compared to females. In a study by Edgar del Toro et al. the prevalence of nasal polyp was 38% in females and 62% in males. [7] Females are more likely to have severe disease as compared to that of males. Histological examination of the polyps show fibrocollagenous tissue covered by pseudostratified ciliated columar epithelium with/without squamous metaplasia. The subepithelial stroma shows oedema, varying degrees of inflammatory cells, reactive fibroblasts, hyperplasia of seromucinous glands, etc. They are divided into various types based on the predominant component which is seen histologically and the classification is as follows but this is not used in routine practice.
Oedematous or eosinophilic polyps: characterised by stromal oedema and moderate inflammatory infiltrates of eosinophils and mast cells.
Fibroinflammatory polyps: characterised by moderate to marked inflammatory infiltrates of inflammatory cells. They lack stromal oedema and goblet cell hyperplasia.
Polyps with seromucinous gland hyperplasia: characterised by hyperplasia of seromucinous glands in an oedematous stroma.
Polyps with stromal atypia: characterised by the presence of bizarre and atypical stromal cells. [8]
Certain nasal polyps can show unusual features like presence of amyloid, atypical stromal cells, etc. that might cause diagnostic dilemma. Presence of atypical stromal cells can cause confusion with other entities like sarcoma, especially rhabdomyosarcoma. Smith et al. was the first to describe 2 cases of antrochoanal polyps with atypical stromal cells. [9] In 1976, Compagno et al. described 14 cases of nasal polyps with atypical stromal cells. The presence of atypical stromal cells is called by various terminologies like stromal atypia, pseudosarcomatous change, mesenchymal cell atypia, etc. Atypical stromal cells are large stellate to spindle shaped atypical cells with hyperchromatic nuclei, prominent nucleoli and bizarre appearing cells. These atypical stromal cells are seen more commonly adjacent to areas of ulceration, fibrosis, haemorrhage, necrosis or vascular thrombosis. Atypical stromal cells are known to be immunopositive for actin and vimentin. They are negative for desmin, myoglobin, GFAP and S-100. In more than 75% of the cases, the atypical stromal cells expressed cytokeratin. Atypical stromal cells are known to represent reactive myofibroblasts. Hence, we need to be aware about the presence of atypical stromal cells in nasal polyps which would otherwise cause difficulty in diagnosis.
Conclusion
Polyps from the nasal cavity and paranasal sinuses are routinely submitted for histopathological examination to look for fungal organisms, allergic mucin and to exclude the presence of dysplasia/malignancy. Though rare, it is important to be aware of the presence of unusual features like atypical stromal cells as they help in preventing an erroneous diagnosis of sarcoma.
Source of Funding
None.
Conflict of Interest
None.
References
- RA Settipane, AT Peters, AG Chiu. Allergic Rhinitis. Am J Rhinol Aller 2013. [Google Scholar]
- WJ Fokkens, VI Lund, J Mullol, C Bachert, I Alobid, F Baroody. EPOS 2012: European position paper on rhinosinusitis and nasal polyps 2012. A summary for otorhinolaryngologists. Rhinology 2012. [Google Scholar]
- JR Newton, KW Ah-See. A review of nasal polyposis. Therapeutics and clinical risk management. Ther Clin Risk Manag 2008. [Google Scholar]
- BSAl Jobran, AE Alotaibi, AY Asiri, RM Alhayyani, RM Alhayyani, NI Almanie. Nasal polyps and its histo-pathological evaluation. Egypt J Hosp Med 2018. [Google Scholar]
- LG Kindblom, L Angervall, . Nasal polyps with atypical stroma cells: a pseudosarcomatous lesion. A light and electron-microscopic and immunohistochemical investigation with implications on the type and nature of the mesenchymal cells. Acta Pathol Microbiol Immunol Scand A 1984. [Google Scholar]
- A Starry, F Hardtstock, T Wilke, J Weihing, B Ultsch, M Wernitz. Epidemiology and treatment of patients with Chronic rhinosinusitis with nasal polyps in Germany-A claims data study. Allergy 2022. [Google Scholar]
- JS Lewis. Spindle cell lesions--neoplastic or non-neoplastic?: spindle cell carcinoma and other atypical spindle cell lesions of the head and neck. Head Neck Pathol 2008. [Google Scholar]
- CJ Smith, R Echevarria, CA Mclelland. Pseudosarcomatous changes in antrochoanal polyps. Arch Otolaryngol 1974. [Google Scholar]
- J Compagno, VJ Hyams, ML Lepore. Nasal polyposis with stromal atypia. Review of follow-up study of 14 cases. Arch Pathol Lab Med 1976. [Google Scholar]
