Introduction
Hemophagocytic lymphohistiocytosis(HLH) is a rare disease and unlikely under-recognised, whichis an emergency to treat the patient as it carries high and fast mortality. The underlying aetiology varies from infections to autoimmune disease and malignancy.1 HLH is classified as familial (primary) which occurs in young children with an incidence of approximately 1.5 per 100,000 live births and acquired(secondary) occurs in old age.2 The familial HLH have association reported with Chédiak-Higashi syndrome, Griscelli syndrome type 2, Hermansky-Pudlak syndrome type 2 and X linked lymphoproliferativedisorder types 1 and 2 and with no association with malignancy.3 Acquired or secondary HLH is more common in older children and adults; its incidence is unknown but is likelyunderdiagnosed.1, 3 No race or sex predilection seen in HLH.There is an excessive amount of cytokines secretion which result in activation and proliferation of macrophages/histiocytes and lymphocytes, leading to multiorgan failure and subsequently death. 4, 5The diagnosis of HLH is solely based on current criteria HLH -2007(updated version of HLH-2004), five out of eight criteria must be met for the laboratory diagnosis. 6, 7The hematological findings of histiocytic hemophagocytosis are predominantly diagnosed in bone marrow aspirate or biopsy, and which is rarely noted in peripheral blood smear. However, when it does appear inperipheral blood smear as circulating histiocytes engulfing blood components,it is typically associated with a high risk of fatality,8 As per the best of our knowledge, only 6 cases of HLH presented as peripheral finding documented online and no case found to report in India. We present an extremely rare case of an adult male from Indiapresented as peripheral circulating hemophagocytic histiocytes being the first clue to arrest the diagnosis of HLH.
Case Presentation
An Indian male in his early 30s, presented to the emergency with complaints of fever on &off and generalised weakness from 1 month and slurring of speech and oligouria since 20 days. On examination, patient was thin built and had fever and palpable spleen. An ultrasound was requested.
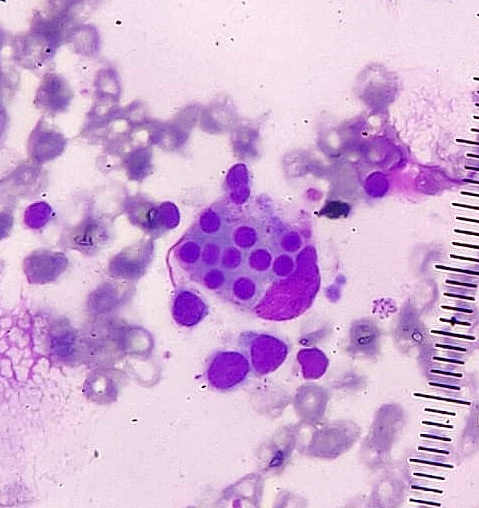
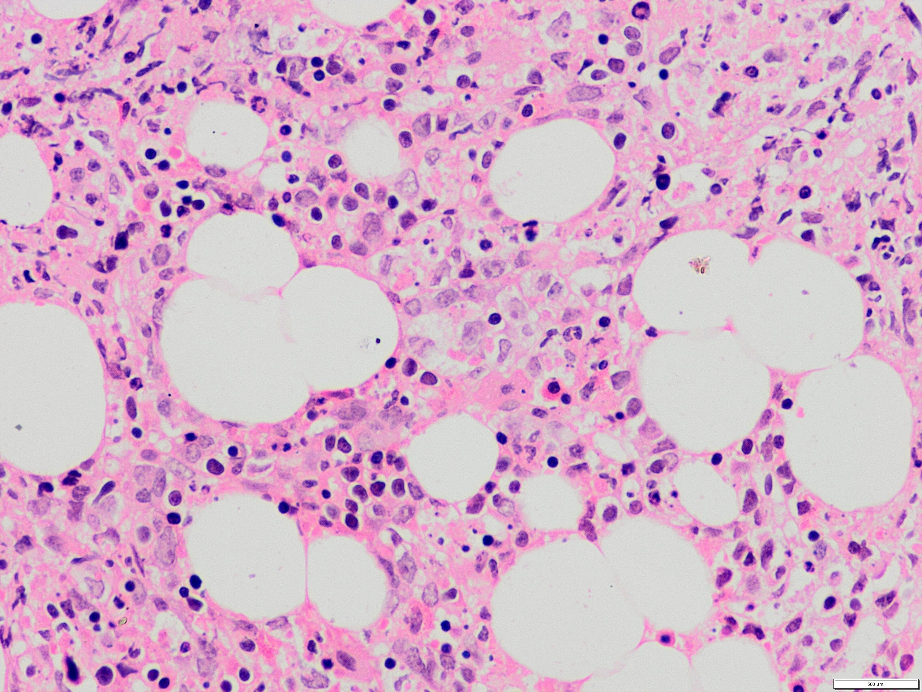
The EDTA sample was received in the hematology lab for complete blood counts(CBC)(Table 1). The CBC showed pancytopenia. The peripheral blood smear(PBS) studied show normocytic normochromic red blood cells (RBCs) along with few immature erythroid precursors. Few histiocytes were noted and all of them showed hemophagocytic activity with engulfed mature RBCs as well as white blood cells(WBC), platelets and debris (Figure 1, Figure 2 ). The following tests were further advised on the basis of this interesting finding, firstly bone marrow examination to rule out possibility of Hemophagocytic activity(Table 1). The bone marrow aspiration was performed resulted in dry tap. Bone Marrow Biopsy was taken and imprint smears were made. Microscopy showed raised histiocytes and almost all histiocytes show features of hemophagocytosis Figure 3, Figure 4].
The patient developed more symptoms within 2 days i.e. acute colicky pain, excessive sweating, delirium, giddiness and progressive weakness. The Ultrasound(USG) report showed hepatosplenomegaly. An ECG done showed PR depression and ST elevation. The Typhidot test came out to be cross-reactive, considered as false positive.
The hematological , serological and bone marrow findings met with the criteria of Hemophagocytic lymphohistiocytosis(HLH), i.e fever, pancytopenia, elevated ferritin & triglycerides, splenomegaly, hypofibrinogenemia and histiocytic hemophagocytosis reported in bone marrow biopsy as well in PBS. Although, the patient succumbed to death the very next day of diagnosis even after the therapy started. The progression of clinical events and appearance of signs and symptoms and formation of diagnosis all happens within 2 days of hospitalisation.
Table 1
Laboratory findings of case reported.
Figure 1
Peripheral blood smear of an Indian male in his early 30s, A histiocyte engulfing a stack of mature RBCs(Leishmans stain, 400 X).
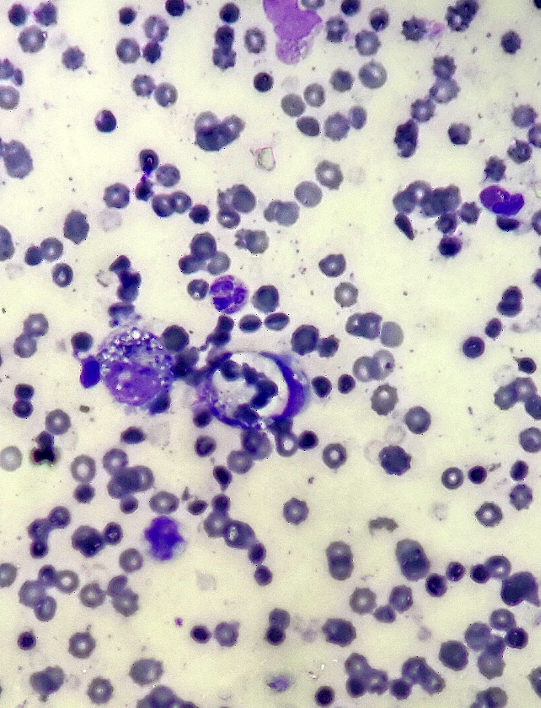
Figure 2
Peripheral blood smear showed large sized foamy histiocytes engulfing platelets and a RBC. A reactive lymphocyte noted with intracytoplasmic granules(Leishmans stain, 400 X).
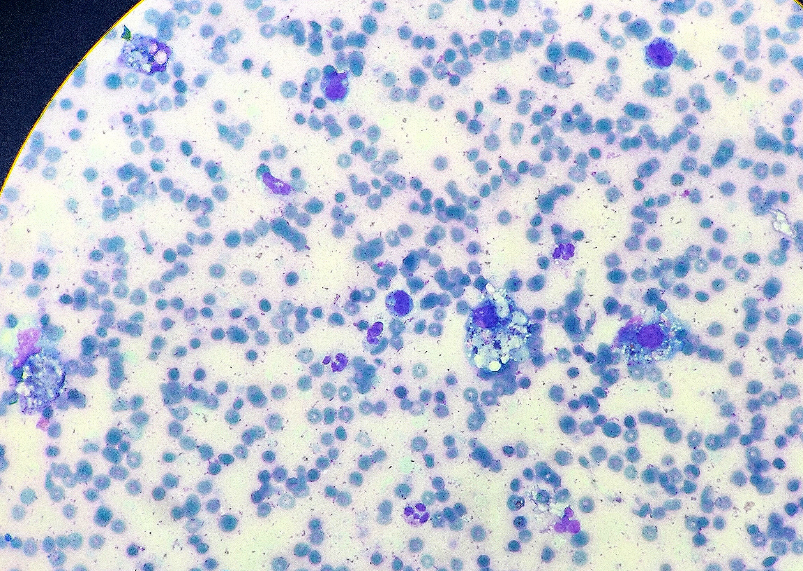
Discussion
Hemophagocytic lymphohistiocytosis(HLH) is a rare disease and unlikely under-recognised, which is an emergency to treat the patient as it carries high and fast mortality. The underlying aetiology varies from infections to autoimmune disease and malignancy.1 HLH is classified as familial (primary) which occurs in young children with an incidence of approximately 1.5 per 100,000 live births and acquired(secondary) occurs in old age. 2 The familial HLH have association reported with Chédiak-Higashi syndrome, Griscelli syndrome type 2, Hermansky-Pudlak syndrome type 2 and X linked lymphoproliferative disorder types 1 and 2 and with no association with malignancy.3 Acquired or secondary HLH is more common in older children and adults; its incidence is unknown but is likely underdiagnosed.1, 3 No race or sex predilection seen in HLH.
Table 2
Case reports with peripheral histiocytic hemophagocytosis world wide.
|
Study |
Age/Sex |
Clinical presentation |
Peripheral Blood Smear findings |
Other Investigations |
Outcome |
|
Sloma et al.8 (2014,Paris,France) |
79yr/ F |
High grade Fever |
Single hemophagocytic histiocyte |
Acute Myeloid leukemia with t(8;21)(q22;q22) , diagnosed in bone marrow aspirate sample |
Patient died after 21 days of admission Azacitidine treatment was given |
|
Lee et al.9 (2019) |
42 days /F |
Fever ,Anemia ,Jaundice, Severe Thrombocytopenia Hepatosplenomegaly |
Leucoerythroblastic picture Atypical Lymphocytosis Neutrophils show toxic granulation Hemophagocytosis |
CRP- 194 mg/L Blood Culture- Serratia Marcescens |
Patient died after 23 days due to rupture of abdominal aortic aneurysm |
|
Brittney Graham et al. 10 (2020) |
66yr/M |
N/A |
Histiocytic Hemophagocytosis |
Newly diagnosed with Diffuse large B cell lymphoma (DLBCL) Bone marrow -Histiocytic Hemophagocytosis |
N/A |
|
Mohammed Al Shariff 11 (2021) |
15 days/F |
Neonatal sepsis , admitted in NICU |
Rare histiocytes with hemophagocytic activity |
|
N/A |
|
Ali et al. 1 (2023, Karachi, Pakistan) |
7 yr/F |
Fever Ventriular Septal Defect (VSD) with MRSA Endocarditis |
No abnormal findings at the beginning On 20th day of hospitalisation, few histiocytes showing hemophagocytic activity of moderate grade (2-5 histiocytes with hemophagocytosis per slide) |
H Score was calculated without fibrinogen levels – 178 points (optiomal cutoff 169) with a 54-70% probability of hemophagocytic syndrome |
Patient died within 24 hours of positive peripheral smear finding |
|
Jaziri et al 12 (2023,Tunisia) |
67yr/M |
Known Diabetic and smoker Presented with chronic bronchitis Past history of hospitalisation and blood transfusion for COVID 19 pneumonia |
Numerous histiocytes with few showing hemophagocytosis engulfing RBCs and platelets |
|
|
|
Raj et al. [Current Study] (2024, India) |
32 yr/M |
Fever generalised weakness, slurring of speech and oligouria since 20days |
Pancytopenia Fair number of histiocytes seen showing hemophagocytic activity engulfing RBCs and platelets Reactive lymphocytes and few nucleated RBCs noted |
Bone Marrow Aspirate- Dry Tap Bone Marrow Biopsy – Hemophagocytosis USG- Hepatosplenomegaly S.Ferritin >2000 ng/mL Triglycerides- 302 .63 mg/dL |
Patient died within 24 hours of PBS findings |
There is an excessive amount of cytokines secretion which result in activation and proliferation of macrophages/histiocytes and lymphocytes, leading to multiorgan failure and subsequently death. 4, 5
The diagnosis of HLH is solely based on current criteria HLH -2007(updated version of HLH-2004), five of the eight criterias must be met for the laboratory diagnosis. 6, 7
The hematological findings of histiocytic hemophagocytosis are predominantly diagnosed in bone marrow aspirate or biopsy, and which is rarely noted in peripheral blood smear. However, when it does appear in peripheral blood smear as circulating histiocytes engulfing blood components, it is typically associated with a high risk of fatality.8
HLH commonly involves all reticuloendothelial organs i.e bone marrow, spleen, liver and lymph nodes and less commonly involves skin, lungs, meninges, cerebrospinal fluid(CSF) and subcutaneous tissue. The first clinical presentation is generally fever and weakness and commonest first sign is hepatosplenomegaly. The diagnosis of HLH is generally confirmed by performing bone marrow to look for histiocytes and hemophagocytic activity that should be required for the correct diagnosis as major criteria as other criteria is quite misleading in the absence of hematogical finding of histiocytic activity. However, the absence of hemophagocytosis in microscopic examination does not exclude out the diagnosis of hemophagocytic lymphohistiocytosis.13
In our case, the first clue came out as incidental finding while screening the PBS to correct the CBC which showed severe anemia, leucopenia and thrombocytopenia. After that, keeping in mind the suspicion of HLH, we talked to clinician and gave critical alert to perform more investigations and call the patient for bone marrow examination. Finally the patient met with the criteria as per HLH-2007. 6, 7
HLH-2004 criteria(updated 2007) include the molecular diagnosis of familial hemophagocytic lymphohistiocytosis or the presence of at least 5 of 8 criteria. 6, 7
Fever
Splenomegaly
-
Cytopenias(affecting at least 2 lineages in the peripheral blood
-
Hypertriglyceridemia or hypofibrinogenemia
Documented hemophagocytosis in the bone marrow, spleen or lymph nodes
Low or absent NK cell activity
Ferritin ≥ 500 μg/L
Soluble CD25 ≥ 2,400 U/mL
We review the literature for case reports of histiocytic hemophagocytosis that showed positive results on PBS and raised suspicions of HLH(Table 2). We were unable to locate any instances of this type that had been reported in India up to this point that raised suspicions of HLH based only on PBS screening. The study showed half cases from pediatric age group and other half from geriatric age group. The female preponderance noted in our group study with fever being the most common symptom and first presentation. Two out of 7 cases presented with newly diagnosed malignancies, one with Acute Myeloid Leukemia(AML) t(8;21)(q22;q22)8 and other with diffuse large B cell lymphoma(DLBCL), 10 both were of geriatric age group. One child presented with congenital heart defect ;Ventricular Septal Defect(VSD) 1 and one patient had co-morbidity, i.e known case of diabetes and also had past history of COVID19 pneumonia. 12 The occurrence of HLH in COVID 19 was previously postulated as cytokine storm. Unfortunately, 4 out of 7 including our case were succumbed to death in 24 hours to 23 days(Table 2), and there is no available data for rest 3 cases.
In our case, patient had slurring of speech might raise a possibility of CNS involvement(meninges) but the CSF examination couldn’t be performed. The cause of death is presumptive of meningitis or multiorgan failure, as renal insufficiency and jam packed bone marrow with histiocytes, and dry tap was noteworthy.
Current treatment regimens available are immunosuppression, immune modulation, chemotherapy, and biological response modification, followed by hematopoietic stem-cell transplant(bone marrow transplant). 4
Conclusion
The diagnosis of hemophagocytic lymphohistiocytosis is urgent and requires immediate evaluation because of its high and early mortality rate. HLH workup should be done if the above-described PBS findings are seen during regular microscopy. It is crucial to keep a high degree of suspicion and use beneficial laboratory tests in compliance with HLH-2007 diagnostic criteria, as well as additional helpful tools like the H score, HLH 2004, and modified HLH 2007. The therapeutic modality must focus on specifically addressing the underlying primary pathology as it may be the root cause, because of huge range of aetiology from infections to malignancy to idiopathic.
Therefore, PBS screening and bone marrow aspiration studies are utterly needed for early diagnosis and management, defining it as the simplest, quickest, least expensive, and most accessible investigation in developing country. Henceforth, meticulous observation and non negligence of PBS findings can be the first clue to arrest the diagnosis of Hemophagocytic lymphohistiocytosis and may serve as the primary and early diagnostic standard.