Introduction
Multiple granulomatous lesions of the prostate have been described with varied etiology and pathogenesis.1 Xanthogranulomatous prostatitis is a rare form of nonspecific granulomatous prostatitis distinguished by presence of xanthoma cells. The most common xanthogranulomatous inflammations are seen in the kidneys and gallbladder. 2, 3 It is uncommon in prostate with very few cases reported in medical literature.4, 5, 6, 7 The age at which patients present can vary. Cases have been reported in patients in their 20s and in the elderly with average age at diagnosis being in early 60s.4, 8 The presentation typically involves lower urinary tract symptoms (LUTS) or symptoms of a lower urinary tract infection (UTI).
Here in we report the case of a patient who underwent Transurethral resection of prostate (TURP) in view of clinico-radiological diagnosis of benign prostatic hyperplasia (BPH). On histopathological evaluation xantho-granulomatous prostatitis was an incidental finding along with evidence of BPH.
Case Presentation
A 56-year-old man presented with a history of difficult urination, decreased flow and retention of urination which was exacerbated from last few days. The patient also had burning micturition. Digital rectal examination (DRE) revealed an asymmetric and enlarged prostate. The patient’s general physical examination was normal, and revealed no alterations of the penis, the testicles or the epididymis. Urine analysis were within normal limits with no growth in urine culture. A transabdominal ultrasonography showed enlarged prostate both in size and volume (approx. 95-100cc). Intravesicular protrusion measuring 2.4 cm was noted in the bladder base with trivial interbowel fluid in pelvis. Urinary bladder wall was also thickened and trabeculated, favoring cystitis.
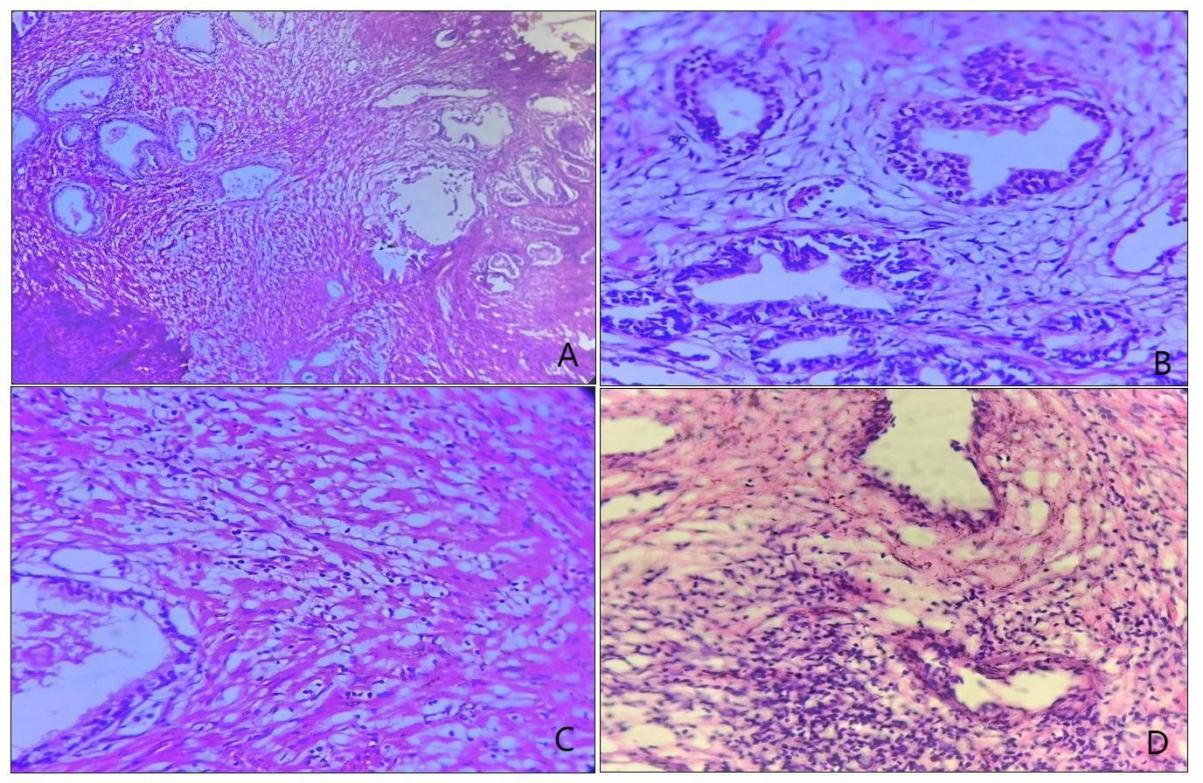
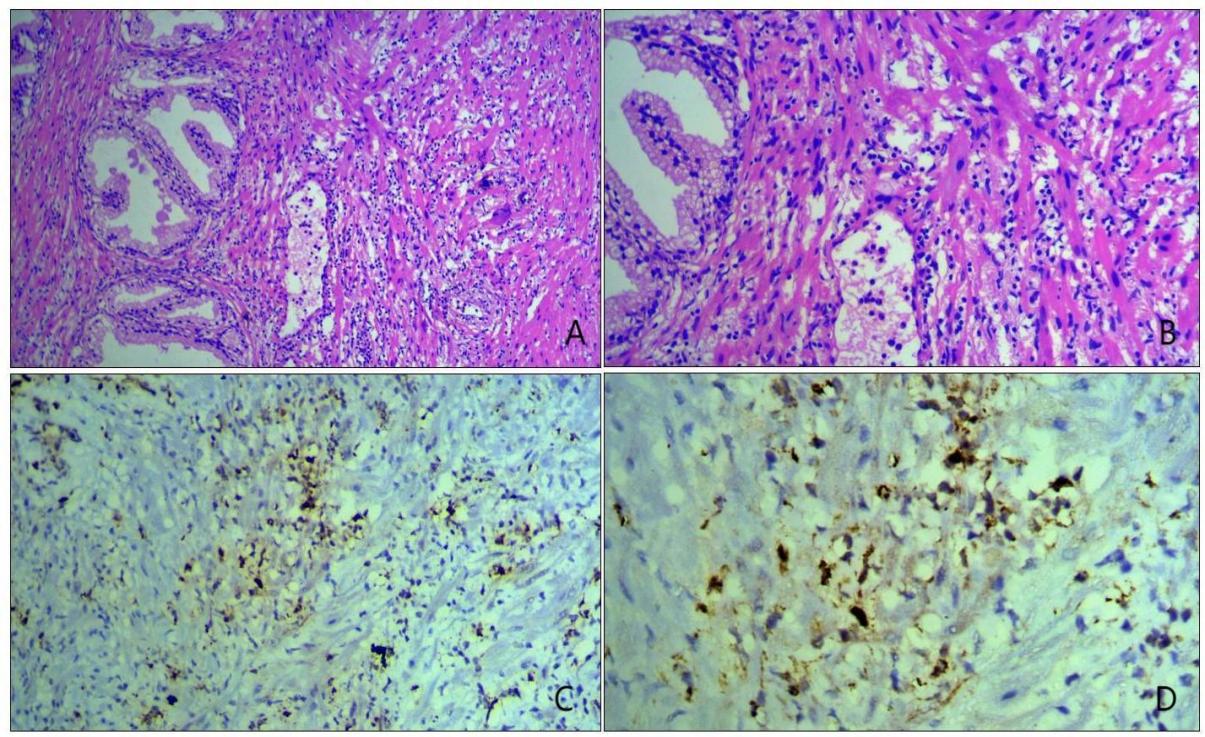
Based on these findings, including progressive LUTS, recurrent urinary tract infections (UTI), and low flow rate, the patient underwent transurethral resection of the prostate (TURP). His intraoperative and postoperative course was uneventful. Prostatic chips were received in 10% formalin and were processed routinely. The slides were stained with Hematoxylin and Eosin. Histopathologic examination of the transurethral resection of the prostate showed hyperplasia of glandular and stromal tissue. Hyperplastic glands were lined by bilayered prostatic epithelium showing papillary infoldings at places (Figure 1, Figure 2).
Few cystically dilated glands are also seen. Intra luminal secretion and corpora amylacea are seen in some of the glands. Stroma shows variable degree of fibrosis, few blood vessels and large number of foamy macrophages which are arranged in sheets as well as in nodule along with chronic inflammatory cell infiltrate (Figure 1, Figure 2). Histiocytes showed positivity for CD 68 (Figure 2 C&D). Based on histomorphological & immunohistochemistry findings, a diagnosis of benign prostatic hyperplasia with xanthogranulomatous prostatitis was made.
Discussion
Granulomatous prostatitis is a relatively rare condition. Variable etiology can be associated with this entity. It can be of infectious tuberculous origin in the context of urogenital tuberculosis or, after BCG therapy, parasitic following non-specific urogenital or bacterial schistosomiasis or mycotic in immunocompromised patients. It can occur after transurethral resection of prostate adenoma or after prostate biopsy.9 Xanthogranulomatous prostatitis is an uncommon form of non-specific granulomatous prostatitis.
Xanthogranulomatous inflammation involving the kidneys and gallbladder is common.3 However, xanthogranulomatous prostatitis is rare.4, 7 The exact cause of xanthogranulomatous inflammation is unknown. 10 It is thought to represent a reaction to inflammatory products and altered prostatic secretions released through clogged ducts. Recently, a study has linked this condition to autoimmune disease. 5, 11 Clinically, the symptoms include a urinary obstruction or a severe infection of the lower urinary tract. 12
In most cases, xanthogranulomatous prostatitis is diagnosed incidentally on TURP chips or needle biopsy.13, 14, 15 Clinically, the symptoms are either those of urinary obstruction, with low grade or high grade urinary tract symptoms. Two recent studies have shown that the most encountered symptoms were increased urinary frequency and urgency, sometimes with dysuria, burning micturition, haematuria and urinary incontinence. 13, 14
Therefore, the diagnosis of xanthogranulomatous prostatitis is made on histological examination of the prostate. 14 The distinguishing feature of xanthogranulomatous prostatitis is the presence of a large number of "foamy macrophages" (histiocytes) in the infiltrate of inflammatory cells. Xanthogranulomatous prostatitis causes serious confusion with prostate carcinoma when it comes to diagnosis. It occurs usually in elderly men, usually in the sixth decade. 13, 14
A panel of immunohistochemistry tests, such as cytokeratin, Prostate specific antigen (PSA), prostatic acid phosphatase (PAP), leukocyte common antigen (LCA) and CD68 can be useful in differentiating between these two conditions, by showing results more consistent with an inflammatory process. 6, 13, 15 We used only CD68 in our case to confirm the presence of foamy macrophages as there was no much discrepancy in our case in evaluating the slides. No evidence of malignancy was there in slides examined. To label the case as xanthogranulomatous prostatis, we utilised this CD 68 IHC.
Inflammation is often self-limiting and resolves slowly over time. Conservative treatment is recommended for xanthogranulomatous prostatitis, including alpha-blockers and corticosteroids. Surgical options, such as transurethral or open prostatectomy, are reserved for patients who have severe symptoms or in whom conservative treatment has failed.
Conclusion
Xanthogranulomatous prostatitis is rare clinical disease, which should be excluded from prostate cancer and can be confirmed by precise histopathologic examination. According to the degree of lower urinary tract obstruction, it is treated by medicine or surgical operation. There are no specific radiological features. Knowledge of this condition and close co-operation with pathologist is necessary for the diagnosis of xanthogranulomatous prostatitis and differentiating it from other mimickers.