Introduction
Phyllodes tumours (PT) account for less than 1% of mammary gland tumours.1 They are biphasic tumours with epithelial and stromal components. PTs are classified as benign, borderline, or malignant.2 Malignant phyllodes tumours account for 10% to 20% of PTs.3 At presentation, 80% are localized. Malignant phyllodes tumour with osteosarcomatous transformation are extremely rare and is often misdiagnosed as benign giant calcifications radiologically. 1 It is an aggressive neoplasm with distant metastasis. Extensive sampling is important because presence of heterologous elements carry poor prognosis. We are presenting a case of malignant PT with osteosarcomatous and liposarcomatous elements.
Case presentation
We present the case of a 64-year-old postmenopausal woman who was diagnosed with plasma cell myeloma in 2016 but defaulted on treatment in 2020. 3 years later in 2023, she again presented with myeloma symptoms, and chemotherapy was restarted. 6 months later, she noticed a lump in the right breast which was gradually increasing in size. There was no family history of malignancy. Physical examination revealed a mass of 5x7cm size in the upper inner quadrant of the right breast. No associated pain, dimpling of overlying skin, nipple retraction, or discharge noted. Computed tomography (CT) revealed an enhancing lesion with calcifications and the tumour did not involve the underlying ribs (Figure 1). No significant regional lymph nodes were noted. Ultrasonography revealed a soft tissue mass with coarse calcifications in the right breast. An Aspiration breast cytology showed features of malignant spindle cell neoplasm. Core biopsy from the lesion was inconclusive. The clinician proceeded with a wide local excision and was sent to the pathology department.
Figure 2
Wide local excision specimen showing ill-circumscribed grey-white firm lesion with cystic spaces

Figure 3
Leaf-like fronds with underlying stromal proliferation (on right) andmyxoid areas (on left). H&E 40x
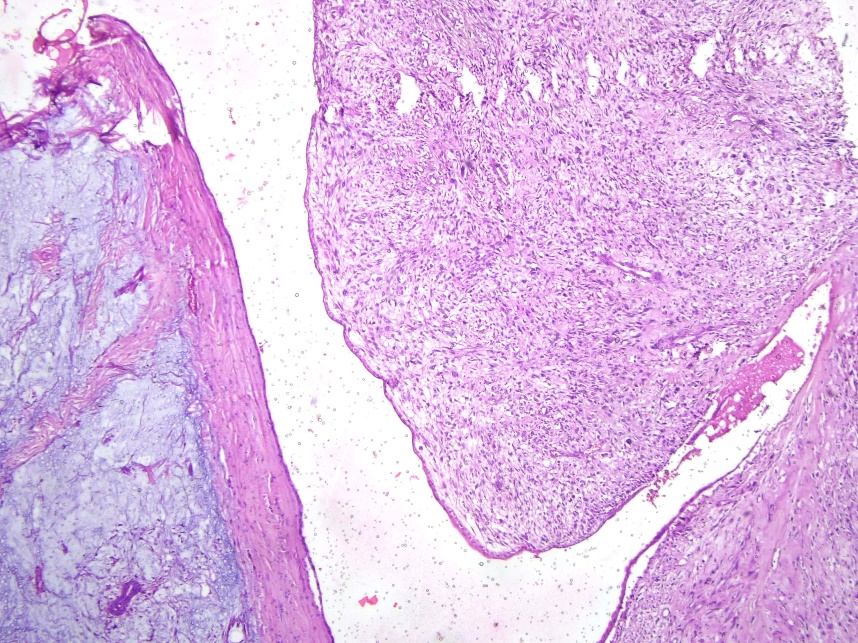
Figure 5
Tumour osteoid with malignant stromal cells (left; H&E. 400x) showing SATB2 positivity (right; 400x)
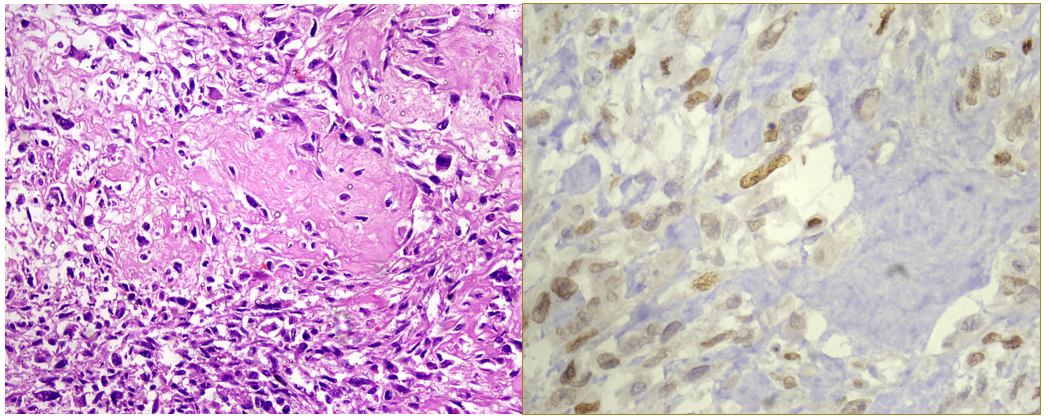
Figure 6
Area of well-differentiated liposarcoma (left; H&E. 100x) showing MDM2 positivity (right; 200x)
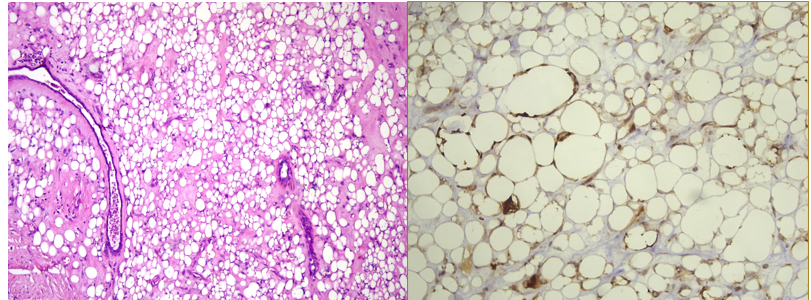
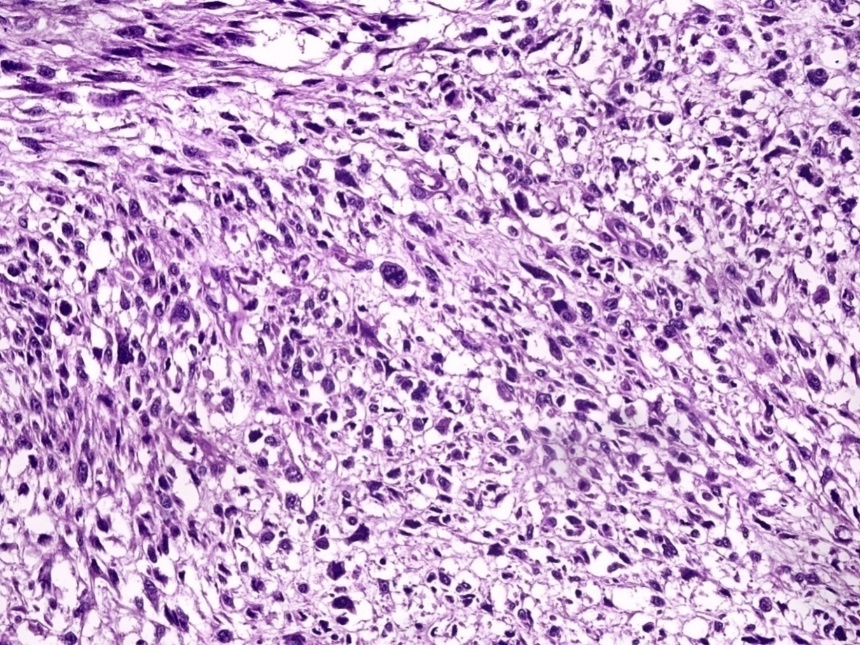
An ill-circumscribed grey-white firm lesion measuring 6.5x6x5.4 cm with cystic spaces containing brown mucoid material was noted on serial sectioning (Figure 2). Histopathological examination revealed an infiltrating neoplasm with stromal overgrowth comprising of markedly pleomorphic spindle cells, and multinucleated and bizarre cells. Leaf-like fronds covered with benign epithelium were also noted (Figure 3). Increased mitoses (>5/mm2) along with atypical mitotic figures present (Figure 4). Myxoid areas were also seen. Focal area with tumour osteoid rimmed by tumour cells was noted which showed diffuse SATB2 nuclear positivity (Figure 5). Another focus showed adipocytes of varying sizes interspersed with atypical spindle cells which were diffusely positive for MDM2 (Figure 6). All margins of surgical resection were free of neoplasm. A final diagnosis of Malignant phyllodes tumour with osteosarcomatous and liposarcomatous components was made.
Discussion
Malignant PT is characterized by increased stromal cellularity, marked stromal pleomorphism, stromal overgrowth, more than 5 mitoses per mm,2 and infiltrative tumour margins.4 Presence of malignant heterologous elements within the tumour such as chondrosarcoma or osteosarcoma directly qualifies PT as malignant. According to the World Health Organisation 5th edition of breast tumours, the presence of a well-differentiated liposarcoma component alone is not considered a malignant component because of low metastatic risk and lack of MDM2 or CDK4 amplification. 5 Malignant PTs with osteosarcomatous component only accounts for 1.3% of PTs. According to Silver et al. they are more aggressive and metastases to the lung, bone, brain, contralateral breast and other distant organs have been reported.6 It is necessary to rule out the possibility of primary osteosarcoma of breast which is characterised by neoplastic osteogenesis or osteoid without epithelial component. Studies have shown that the risk of metastasis of malignant PTs with osteosarcomatous differentiation is substantially lower than that of conventional osteosarcomas in general.7 Malignant PTs should be differentiated from metaplastic carcinoma of breast when a predominant component of atypical spindle cells is noted. This distinction is critical because the treatment and prognosis differ significantly.8
Several studies have shown a correlation between radiologic findings and the histological grade of PTs.9 However, a thorough pathological examination is crucial for grading PTs and identification of heterologous elements.
Currently, the patient is on chemotherapy for plasma cell myeloma and under follow up for malignant PT. A possibility of second malignancy to primary hematological malignancy can be considered in this case. Development of hematological malignancies and solid malignancies like carcinomas of breast, lung, colon and prostate has been reported following chemotherapy for myeloma. To the best of our knowledge, secondary malignant PT has not been reported. Hence, we think that this is the first reported case.