Introduction
Granulomatous gastritis (GG) is a rare pathological finding that accounts for only 0.08-0.35% of all gastric biopsy samples, which is characterized by granulomas within the gastric mucosa or submucosa.1 Granulomatous gastritis is classified as infectious, non-infectious, and idiopathic GG based on etiology. The most common causes of GG in developed countries are Crohn’s disease and sarcoidosis. Infections are the most encountered causes of GG in resource-limited countries mainly tuberculosis. Parasitic infections, Whipple’s disease, foreign body reaction and adenocarcinoma are the rare causes of GG.1 Identifying the cause of GG requires a clinical, endoscopic, and histopathological evaluation. 2 This report describes two surgical cases of Granulomatous gastritis, diagnosed by histopathological examination of the gastric tissue taken by biopsy.
Case History
Case 1
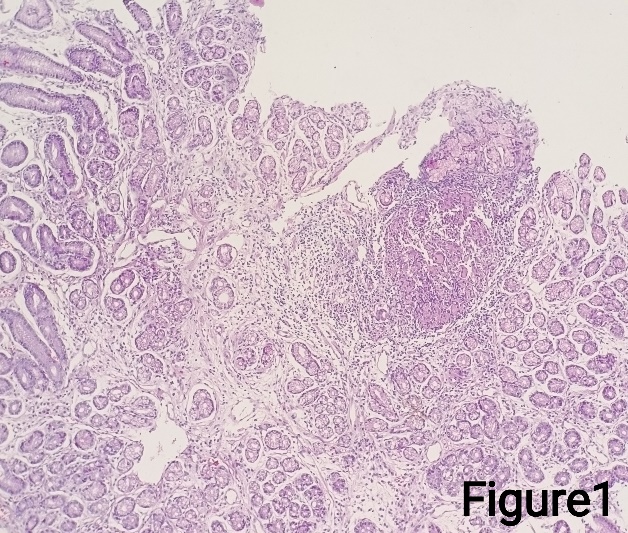
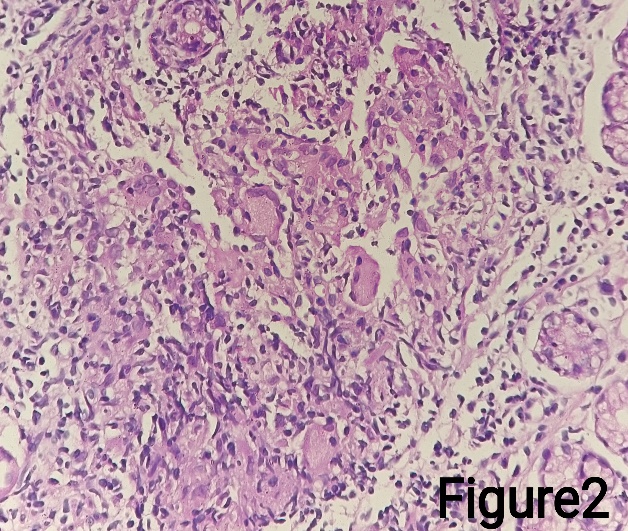
A 40-year-old male presented with complaints of abdominal pain on and off for the past six months which was pricking in nature, intermittent in type, radiating to the back and bilateral shoulders. No specific aggravating factors were found. No change in the pain before or after food, relieved on lying down and after taking medication. He had no complaints of fever, nausea, vomiting, loose stools, constipation, hematemesis, dyspepsia, or weight loss. He had a history of smoking and drinking alcohol for 15 years. Vital signs were normal. The abdominal examination revealed soft on palpation with tenderness over the epigastric, left hypochondriac and lumbar regions. All baseline investigations were done. His chest radiograph was normal. The abdominal ultrasonography revealed a bulky pancreas in the region of the head and neck. UGI scopy was done and showed antral and fundal gastritis with duodenitis. During UGI scopy, the biopsy was taken from the antrum and sent for histopathological examination. Grossly we received 3 grey-white soft tissue fragments each measuring 0.3 cm. All were embedded in 1 block, processed and stained with Hematoxylin and eosin. Microscopically, the representative sections revealed multiple fragments of gastric mucosa and lamina propria showing edema and inflammatory cell infiltration of lymphocytes and plasma cells. Few eosinophils and neutrophils with mild activity and focal lymphoid aggregates were noted (Figure 1). Upon higher magnification, one fragment revealed an aggregate of epithelioid cells forming granuloma with Langhan type of giant cells (Figure 2). No evidence of atrophy/intestinal metaplasia/necrosis/dysplasia/H.pylori organism in the material received. Special staining with Giemsa and Ziehl-Neelsen stain was done which were negative for H. pylori and acid-fast bacilli.
Case 2
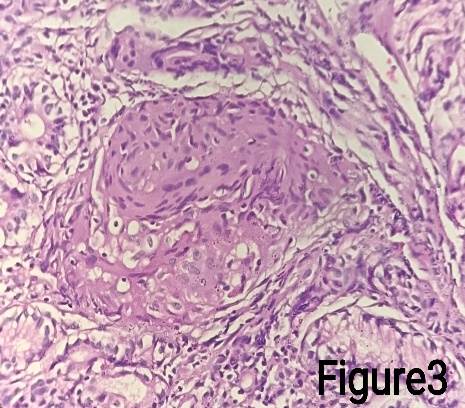
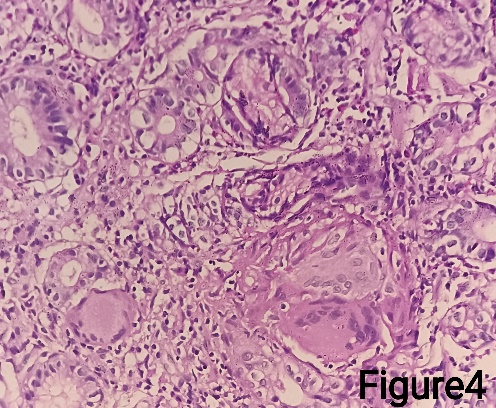
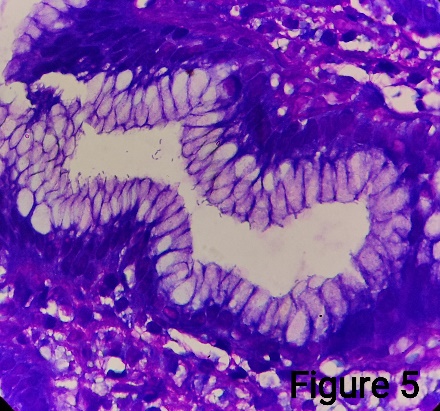
A 43-year-old female presented to the gastroenterology department with complaints of abdominal pain, diarrhoea, and weight loss for three months without any history of fever, nausea, vomiting, constipation, rectal bleeding, and malena. There was no history of tuberculosis in her family members. Her vital signs were normal. The general examination was also insignificant. The abdominal examination revealed tenderness over the epigastric region. Laboratory investigation revealed haemoglobin of 7.2 g/dl (microcytic hypochromic anaemia) with normal WBC and platelet counts. She had a normal chest radiograph and abdominal ultrasonography. Her electrolytes, creatinine, calcium, renal and liver function tests were normal. Upper GI scopy showed an ulcerated lesion and hyperemia in the antral mucosa and nodule at the pylorus of the stomach. During UGI scopy, biopsies were taken from the antrum and pyloric mucosa and sent for histopathological examination. Grossly, we received two grey-white soft tissue fragments each measuring 0.5 cm in one container and four grey-white soft tissue fragments each measuring 0.5 cm in another container. Microscopically, sections from the antral biopsy showed antral mucosal glands with severe activity and positive for H.pylori which was further confirmed by special staining with Giemsa (Figure 5). Another section from the gastric mucosa showed numerous epithelioid granulomas with few Langhan type of giant cells and chronic inflammatory cells within the lamina propria (Figure 3, Figure 4). No necrosis or dysplasia were seen in the sections studied. Ziehl-Neelsen stain was negative for acid-fast bacilli.
Discussion
Granulomatous gastritis is an uncommon inflammation pattern, characterized by non-necrotizing epithelioid cell granulomas.3 The most frequent location of granulomas is the antrum and more prone to cause damage within the pits where the H.pylori organisms commonly reside. These findings indicate that H.pylori can be responsible for the pathogenesis of granulomatous gastritis.4 GG must be distinguished from infections such as tuberculosis, fungal infections (mycosis), sarcoidosis, Crohn’s disease, any underlying malignancies, or foreign bodies. When the cause of the inflammation cannot be ascertained, the term Idiopathic granulomatous gastritis (IGG) can be used.5 Granuloma is a rare feature that is mostly seen in granulomatous diseases like Crohn’s disease, sarcoidosis, infections, neoplasms, and vasculitis.6 H.pylori may be accountable in rare cases, if so, then the patients must be evaluated and treated. The association between H.pylori and GG was first reported in the year 1989.7 Miyamoto et al. also reported two cases of granulomatous gastritis associated with H.pylori infection that completely resolved after successful eradication therapy for H.pylori.1 H.pylori seems to be a bacteria with flagella and this causes injury to the gastric mucosa due to flagella motility by persistent immune stimulation from the chronic granulomatous inflammation.6 The formation of a giant fold in fundus and corpus of the stomach may be a consequence of high-grade active H.pylori gastritis. Identifying and eradicating the infection in such cases not only improve the findings related to gastritis but also helps in the regression of giant folds. Therefore, H.pylori associated with granulomatous gastritis is considered as the most important cause.6 Gastric tuberculosis should always be considered when dealing with granulomas in endemic areas.8 As a conclusion, we have reported two cases of granulomatous gastritis in this article. One of which was associated with H.pylori in the antrum of the gastric mucosa. H.pylori eradication therapy for patients suffering from granulomatous gastritis in association with H.pylori infection can help to prevent further complications. It must be differentiated from Crohn’s disease because of similar clinical and endoscopic features. The possibility of Sarcoidosis also should be considered. Combining morphological features with clinical and laboratory investigations will be a useful tool in the diagnosis of GG.