- Visibility 139 Views
- Downloads 8 Downloads
- DOI 10.18231/j.jdpo.2022.044
-
CrossMark
- Citation
Subleukemic leukemia presenting as pancytopenia in an elderly female with mild constitutional symptoms: A rare case report
- Author Details:
-
Mazhar Fahim
-
Naba Hasan
-
Mohammad Adil
-
Kafil Akhtar *
Introduction
Subleukemic leukemia is characterized by the presence of atypical or abnormal white blood cells in peripheral blood with total leukocyte count in within normal range.[1] The risk factors of this rare leukemic condition include ionizing radiation, drug intake like chroamphenicol, nitrogen mustard, chlorambucil, procarbazine, melphalan, cyclophosphamide, phenylbutazone, genetic disorders like Down syndrome, Fanconi Anemia, Ataxia Telangiectasia, Bloom Syndrome and Li-Fraumeni Syndrome.[2] Chloramphenicol treatment can lead to a common form of anemia called hypoplastic anemia, but they rarely progress to leukemia. Though the transition into acute myeloid leukemia has been explained, the mechanism by which chloramphenicol damages the marrow is not clear although it is known to inhibit protein synthesis by binding to the 50S ribosomes.[3] Other etiological features are bacterial causes, viral diseases, malignancy, liver diseases and iatrogenic causes.[4]
The clinical features are nonspecific and include fever, fatigue, weight loss, vague bone pain, bruising or bleeding.[5] Hepatomegaly and splenomegaly may also be seen.[6] On examination tachypnea, tachycardia, pallor, ecterus, edema and lymphadenopathy are commonly encountered. [7]
Case Summary
A 55 years female presented to the Medicine Out Patient Department with complaints of generalized weakness, easy fatiguability and loss of appetite for the past 3 months. There was no history of fever, weight loss, chronic blood loss, worm infestation, radiation exposure and bone pain. She was a non-smoker and did not have any history of chronic illness like diabetes mellitus and tuberculosis.
There was no history of bone marrow suppressant drug or NSAID intake. There was no similar history in the family which suggested any type of genetic abnormality like thalassemia, Hb E disease or hemophilia.
On examination moderate to severe pallor, tachycardia and dyspnoea were observed. There was no hepatosplenomegaly, lymphadenopathy, bone tenderness, petechial rash, glossitis and angular stomatitis.
Chest X-ray was normal and ultrasonography did not reveal any remarkable findings. CT- scan abdomen did not show any organomegaly.
At presentation complete blood count was done which showed hemoglobin of 4 gm/dl, total leukocyte counts of3900/mm,[3] platelet count of 9000/mm3. Coomb’s direct and indirect test was negative. Liver function test result was within normal range, except unconjugated bilirubin which was 1.3 mg/dl. The patient was evaluated for G6PD deficiency which was normal.
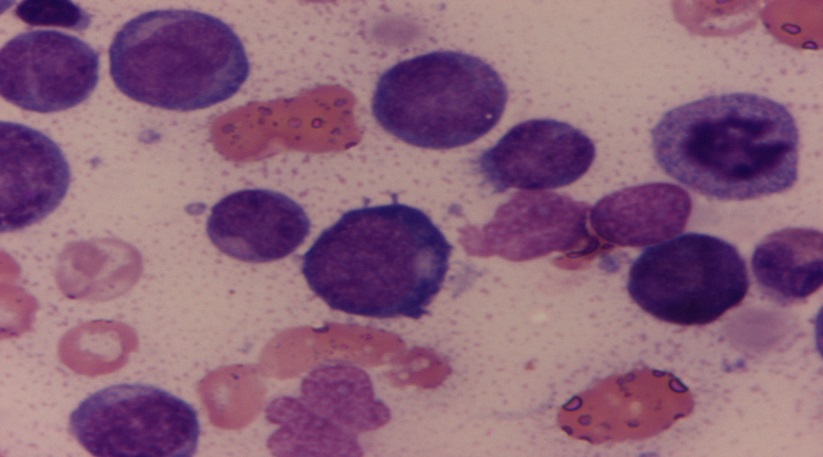
General blood finding findings showed microcytic, moderate to severely hypochromic red blood cells with decreased total leucocyte count. The differential showed 40% immature/atypical cells comprising of 22% myeloblast, 2% myelocytes, 1% promyelocyte, 1% metamyelocyte and 14% stab cells ([Figure 1]).

Blastic precursors were large cells with oval to irregular nucleus with coarse granular chromatin with 1-2 prominent nucleoli and scant granular blue cytoplasm ([Figure 2]). Platelets were inadequate as assessed by the smear.
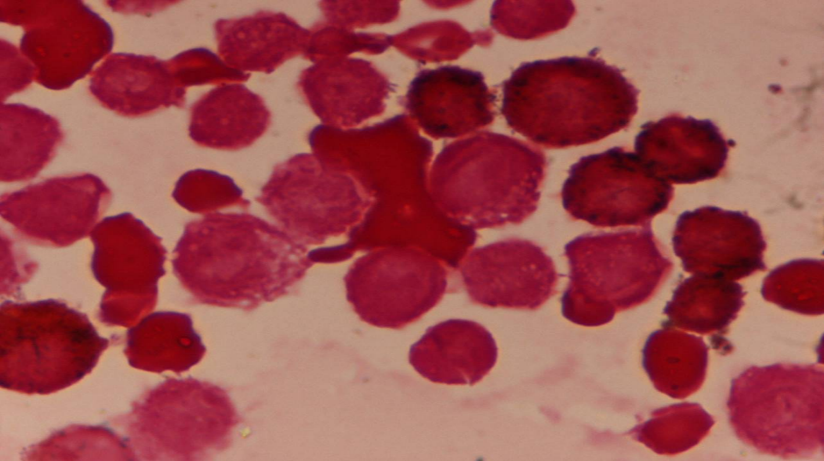
Cytochemical stains MPO and PAS stains were applied for typing of the blasts. MPO showed faint cytoplasmic positivity in few blasts ([Figure 3]) and PAS was negative.
Diagnosis of Acute Leukemia favoring Acute Myeloid Leukemia was given
Two units of packed RBCs, five units of random donor platelet, one single donor platelet were transfused. Mild improvement in haemoglobin and platelet count was noticed after the transfusion but the count again began to deplete. Work up for hemolysis was performed which were inconclusive. She was further transfused 2 units of PRBC’s and subjected to 6 cycles of chemotherapy comprising of 4 drug regimen of cytarabine, daunorubicin, mitoxantrone and methotrexate. She tolerated the drugs well and is fine at 6 months of follow up period with recovery and normalization of her hemopoietic parameters.
Discussion
Subleukemic leukemia is diagnosed when total blood leukocyte count is within normal limit but peripheral blood smear shows few abnormal or atypical cells. [8]
The general clinical features includefever, generalised weakness, bleeding and bone pain.[5] Desalphine et al. in 2014 studied the role of bone marrow aspiration and biopsy to evaluate the cause of pancytopenia and in their study patients' age ranged from 6 to 45 years. The ratio of men to women was 2.5:1. Fever (100%) and weakness (42.8%) were the two most typical presenting symptoms. Pallor (100%) and hepatosplenomegaly (87.5%) were the most often observed physical examination findings. 14.3% of individuals experienced lymphadenopathy. [9]
D'costaet al in 1989 studied pattern of leukemia in 242 cases and observed 53 cases were of subleukemic leukemia and incidence was equal for both AML and ALL, 13 cases for each. [5] Sangwan in 2018 studied 95 cases of pancytopenia and observed three patients with subleukemic leukaemia, ranging in age from 4 to 30 with an incidence of 3.15 percent. Two cases were diagnosed as B-ALL and one case was of AML.Blasts varied from 34 to 43 percent in each of the three cases. [10]
Sharma et al. in 2017 observed11 percent cases of subleukemic ALL, and 4 percent cases of subleukemic AML as the disease progressed that caused pancytopenia in the peripheral blood. They reported that subleukemic ALL was third most common cause of pancytopenia and subleukemic AML the fourth most common cause of pancytopenia.[11] Gupta and Khajuria et al. in 2015 reported subleukemic leukemia as third most common cause of pancytopenia with 6% incidence. They also observed lymphadenopathy in all the three cases of subleukemic leukemia with hepatomegaly in 2 cases and splenomegaly in 1 case. [6]
Rao in 2011 observed four patients with subleukemic leukaemia ranging in age from four to thirty years were having thrombocytopenia and the incidence was 3.85 percent. Three cases of AML-M2 and one case of ALL-L2 type was seen. In each case, the bone marrow was hypercellular. The hematological parameters like haemoglobin was between 2.8-6 mg/dl, total leukocyte count was between 600-3200 cells per cubic millimeter and platelet was between 15,000-85,000 per cubic millmiter. [12]
Agrawal et al. in 2021 studied 65 cases of pancytopenia and observed 4 cases of subleukemic leukemia with an incidence of 6.15 percent.[13] Kumar et al. in 2018 observed 2 patients of subleukemic leukeima presenting as pancytopenia with an incidence of 0.9%.[14] Khunger et al observed 5 percent cases of subleukemic leukemia in their study.[15] Jyoti et al. in 2019 studied 166 cases of pancytopenia and observed 15 cases of subleukemic leukemia and aleukemic leukemia of which ALL was seen in 9 and 6 cases were of AML. In 8 out of 15 cases peripheral blood smear showed blast counts between 3-20 % and rest of the cases belonged to aleukemic leukemia.[16]
Desalphine et al. in 2014 studied the role of bone marrow aspiration and biopsy to evaluate the cause of pancytopenia and observed seven patients of subleukemic leukemia with prevalence of 14 percent. In their study, five of the seven patients had AML, and the two had ALL.[9] Ingale et al. in 2013 described the peripheral blood smear findings in subleukemic leukemia which revealed an increase number of blast cells primarily monoblast and myeloblast in myeloperoxidase staining.[17] Shingade et al. in 2016 did bone marrow evaluation in leukemic patients and observed 2 cases of subleukemic leukemia, with incidence of 3.17 percent. All their cases were of AML M2 type. [18]
Mandal et al. in 2018 observed renal tubular acidosis as complication of subleukemic leukemia in his study on a 7-year-old boy with a seven days history of fast breathing, polydipsia, polyuria, weight loss and history of blood transfusion twice in the past 4 months.[7] Meyer and Boxer in 1973 reported fatality in subleukemic leukemia due to vascular obstruction by leukemic cells. [3]
The treatment protocol of subleukemic leukemia include 21 day regimen of cytosine arabinoside. It is advised to administer along with corticosteroids to prevent depression, malaise and appetite loss associated with cytarabine medication. [17] Prompt supportive care with medicines is advisable to stop and prevent infection. Chemotherapy is frequently used to reduce the amount of aberrant blood cells or to promote the growth of normal cell lines.[18]
Conclusions
We should be aware of this rare finding of subleukemic leukemia in patients with mild constitutional symptoms and keep it in the differentials of a case of pancytopenia, for prompt diagnosis and early initiation of treatment, with better outcome.
Conflict of Interest
The authors declare no relevant conflicts of interest.
Source of Funding
None.
References
- V Buechner, C Zhang, J Robertson, NC Jain, DF Antczak, BF Feldman. Intravascular leukostasis and systemic aspergillosis in a horse with subleukemic acute myelomonocytic leukemia. J Veterinary Internal Med 1994. [Google Scholar]
- M Belson, B Kingsley, A Holmes. Risk factors for acute leukemia in children: a review. Environ Health Perspect 2007. [Google Scholar] [Crossref]
- J S Meyer, M Boxer. Subleukemic myelogenous leukemia following chloramphenicol induced aplastic anemia. Cancer 1973. [Google Scholar]
- K Sawalha, PT Sobash, GR Kamoga. A Rare Cause of Drug-Induced Pancytopenia: Trimethoprim-Sulfamethoxazole-Induced Pancytopenia. Clinics and Practice 2021. [Google Scholar] [Crossref]
- G D'Costa, HM Siddiqui, RM Pradhan, SS Gupte. Pattern of leukemias: a ten-year incidence study of 242 cases. J Postgraduate Med 1989. [Google Scholar]
- N Gupta, A Khajuria. A Clinico-Haematological Evaluation and Correlation with Bone Marrow Examination. JK Science 2015. [Google Scholar]
- P Mandal, N Parakh, P Singh, A Seth, J Chandra. An Unusual Cause of Renal Tubular Acidosis-Subleukemic Leukemia. Pediatri Hematol Oncol J 2018. [Google Scholar]
- K Satué, JC Gardon, M Juzado. A review of current knowledge of myeloproliferative disorders in the horse. Acta Vet Scand 2021. [Google Scholar] [Crossref]
- M Desalphine, PK Bagga, PK Gupta, AS Kataria. To evaluate the role of bone marrow aspiration and bone marrow biopsy in pancytopenia. J Cin Diagn Res 2014. [Google Scholar]
- S Sangwan, Q R Code. A clinico-hematological study of 95 cases of pancytopenia in a tertiary care hospital in India. Platelets. International J Biomedical and Advance Research 2018. [Google Scholar]
- N Sharma, P K Bhatia, K K Kaul, S Sharma, M Sharma. A clinico-hematological study of pancytopenia: An experience of a tertiary care teaching hospital Jammu India. Indian J Pathol and Oncol 2017. [Google Scholar]
- KS Rao. Pancytopenia: a clinicohematological study. J Lab Phys 2011. [Google Scholar]
- P Agrawal, Y Singh, N Agrawal. Haematological Evaluation in Patients of Pancytopenia by Bone Marrow Aspiration. J Evolution Med Dental Sci 2019. [Google Scholar]
- V Kumar, M Khare, M Kishore, M Sharma, S Marwah, AS Nigam. Diagnostic approach of new-onset pancytopenia: study from a tertiary care center. Ann Pathol Lab Med 2018. [Google Scholar] [Crossref]
- J M Khunger, S Arulselvi, U Sharma, S Ranga, V H Talib. Pancytopenia-A Clinico- haematological study of 200 cases. Indian J Pathol Microbiol 2002. [Google Scholar]
- S K Jyoti, B A Badhe, T K Dutta, J Sajjan. of Clinicopathological Study of Adult Pancytopenia with Special Reference to Bone Marrow Biopsy. Int J Blood Disorder Dis 2019. [Google Scholar]
- Y Ingale, T Patil, P Chaudhari, S Routray, M Agrawal. Granulocytic sarcoma of parotid gland in a 4-year-old child with subleukemic AML: a diagnostic challenge!. Case Rep Otolaryngiol 2013. [Google Scholar] [Crossref]
- M S Shingade, R N Shah, A R Sontakke, S C Puranik. Bone Marrow Evaluation of cases of Leukemia in Pathology Department. Indian J Basic Appl Med Res 2016. [Google Scholar]
