Introduction
Salivary glands are distinctive amongst the secretory glands, with most heterogeneous group of tumors, exhibiting complex and wide histological diversity.1 These are exocrine in nature categorized into major and minor salivary glands. Tumors arising from salivary glands, constitute approximately 1% of all neoplasms in the body and 3–6% of all head and neck tumors with an estimated worldwide incidence of 0.4– 13.5 per 1,00,000 population. 2, 3 About 70 - 80% of tumors arise from parotid gland, 7- 10% are located in submandibular gland, the remaining are in sublingual and other minor salivary glands.4, 1 Tumors that arises from parotid, only 15-30% are malignant. More than 50% of those arising in the submandibular or sublingual glands are malignant. 5
Salivary glands are tubuloacinar exocrine organs responsible for production of saliva. 2 Mucins are main component of saliva composed of complex carbohydrates with sugar moieties and amino acids. 6 Glandular secretions protects the mucosa of the oral cavity which are mainly serous and mucinous in nature rich in mucosubstances. 7 Any change in mucin pattern may induce disease or malignant process. Mucin can be are categorized into acidic (sulphomucin and sialomucins) and neutral mucins stained by various methods such as periodic acid schiff (PAS), mucicarmine, alcian blue (AB) and in combination. 6, 8
Hematoxylin and Eosin (H&E) is considered to be the gold standard in diagnosis of salivary gland tumors. Most patients with benign tumors present with painless swelling of the gland involved. Neurological signs, such as numbness or weakness caused by nerve involvement, indicate a malignancy. The prognosis is most favorable when the tumor is located in the parotid gland, 2nd favorable site been submandibular gland, the least favorable sites are the sublingual and minor salivary glands.[2.9]2, 9
Material and Methods
It is a Prospective observational study. salivary gland specimen received at Department of pathology, done at our tertiary care center between November 2018 to June 2021 were taken for the study. Ethical committee clearance was obtained before the study.
Exclusion criteria
All autolytic samples.
Inflammatory, infective and miscellaneous condition.
Salivary gland specimens were obtained after written and informed consent. Details of clinical data and investigations performed collected for available cases from histopathological requisition form. All specimen were fixed in 10% Formalin for a period of 10 – 12 hours. Specimens gross and cut surface examined for size, shape, color, circumscribed or infiltrative borders and presence of cystic changes were noted. The sections were taken from the lesion, its margins, surrounding tissues.
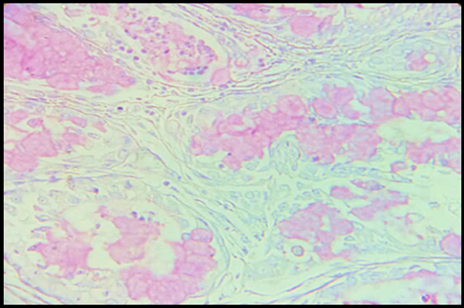
Tissues were processed, embedded in paraffin and sections were cut at 3-5 microns thick and were stained with Haematoxylin and Eosin. Selected cases special stains like Periodic acid Schiff (PAS), Alcian blue (AB) and Mucicarmine (MC) stain were also done, slides were examined. The details of cellular pattern, encapsulation, perineural and vascular invasion with mucin staining pattern was observed. The tumors were studied according to World Health Organization’s histologic typing of salivary gland tumors 4th edition.
Results
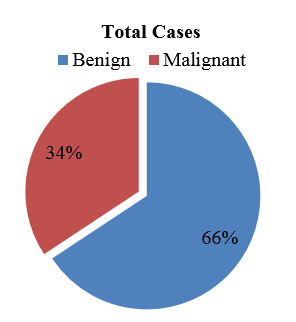
Of the total 70 cases (Table1), of which 46 cases were benign and 24 cases were malignant (chart1).
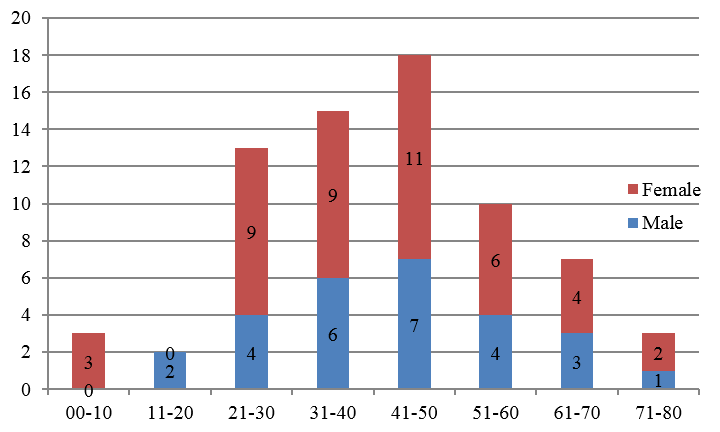
As depicted in Figure 1 Salivary gland neoplastic lesions, tumors were presented over a wide range. The mean age for benign tumor was 43.39 years, malignant tumor was 49.95 years. In this study the youngest patient was 1 year and the eldest was 71 years of age.
Over all female preponderance was observed with ratio of 1:6. Among the benign lesions ratio observed was 1:1.5. M:F ratio in malignant lesion observed was 1:1.6 (Figure 4).
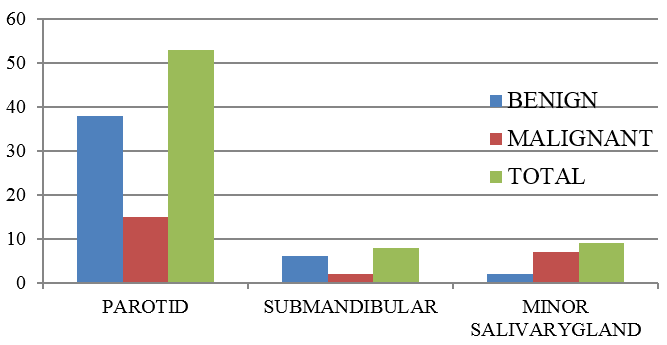
Most common site of benign and malignant salivary gland tumor is parotid with 38 and 15 cases respectively. Second most common site for benign lesion was submandibular gland with 6 cases, but in case of malignant lesion it was minor salivary gland with 7 cases (Figure 3)
Figure 1
Microphotograph of PA showingductal structures surrounded by chondromyxoid stroma with, inset Alcian blue stain shows positive chondromyxoid areas (H&E, 40x and AB, 40x)
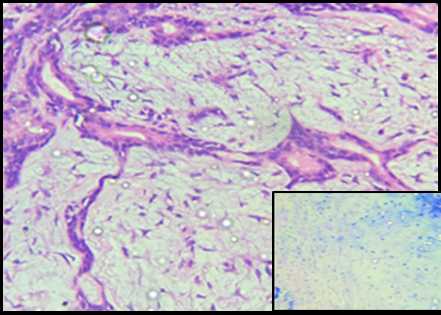
Figure 2
Mucoepidermoid Carcinoma: Microphotograph showing three types of cells: squamous cells, intermediate cells and mucin producing cells. Inset perineural invasion (H&E, 40x)

Figure 3
Mucoepidermoid Carcinoma: Microphotograph showing cyst lining with numerous mucous cells containing mucin pools and is PAS positive (PAS, 10x)
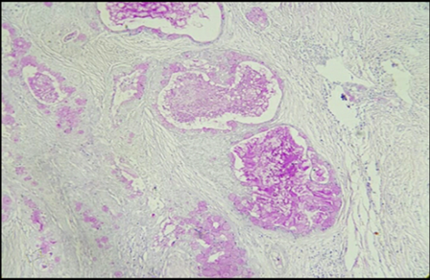
Figure 5
Acinic cell carcinoma: Microphotograph showing large polygonal cells with basophilic granular cytoplasm, round, nuclei. Inset acinar cells are PAS positive (H& E, 40x and PAS 40x)
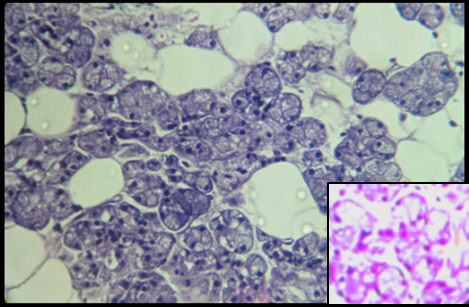
Figure 6
Adenoid cystic carcinoma: Microphotographshowing basaloid cells arranged in tubules and cribriform pattern with cyst like spaces. Inset shows PAS positive material (H& E, 10x and PAS 40x)

Table 1
Percentile distribution of benign and malignant Salivary gland lesion
Discussion
Present study frequency of occurrence of benign tumors were more common when compared to malignant tumors similar results were noted in studies done by Krishnaraj Subhashraj,10 Vargas et al, 11 Amin et al, 12 Ito et al 13 and Bobati et al. 2 The peak age incidence was in the 4th decade for both benign and malignant lesions. The mean age of benign tumor was 43yrs and for malignant tumor was 45yrs the present study correlates with Krishnaraj subharaj,10 Bobati et al. 2 Satko et al 14 had slight higher average age of presentation.
There was female preponderance in both benign and malignant tumors, similar to other studies. However Ahmed et al 15 have observed a male preponderance and Bobati et al 2 showed equal male female ratio in malignant lesions. Parotid was commonest site was seen in present study and correlated with other studies. Second most common site in our study is minor salivary gland similar to the studies done by Ito et al, 13 Krishnaraj Subhashraj. 10 Other studies done by Thomas et al, 16 Ahmed et al 15 showed submandibular gland as second most common site. Thomas et al, 16 Krishnaraj Subhashraj 10 showed least cases in sublingual gland, present study had no cases in sublingual gland similar to Ito et al 13 and Ahmed et al. 15
The PAS stain showed a strong reaction with the mucinous material in the tubules and myxoid arrears. Alcian blue stain was positive for chondromyxoid areas in Pleomorphic Adenoma. These result were similar to the studies done by Naag et al 6 and Azzopardi and Smith. 17 The mucous cells and lumen of MEC showed positivity to MC PAS and AB indicating presence both sulphomucins and sialomucins similar results were observed by naag et al. 6 One rare case was encountered in the study which was clear cell variant of MEC with positive to only PAS stain similar to results was made by Ogawa et al.18 AdCC showed positive for PAS and AB similar result was obtained by naag et al. 6 While ACC showed PAS positive granules were seen in the cytoplasm of the tumor cells.
Conclusion
Parotid gland is the most frequently involved gland by salivary gland tumors. Most commonly presented in middle to older age group. Salivary gland tumors both benign and malignant are more frequent in females. Pleomorphic adenoma is most common salivary gland tumor Mucoepidermoid carcinoma is the most common malignant salivary gland tumor Very less literature is available on the mucin histochemistry of salivary gland tumors. Mucin stain acts as an adjunct to the routine H and E staining. Histopathological examination is gold standard method for diagnosis, predicting prognosis of malignant neoplasms of salivary gland.