Introduction
Nose is the most prominent part of face having great aesthetic value and functional significance. 1 The nasal cavity and paranasal sinuses – including the maxillary, ethmoid, sphenoid, and frontal sinuses are collectively referred to as the sinonasal tract. 2 Due to its prominent position anatomically, it becomes critical to diagnose and treat any scarring or ulceration as early as possible. Filtering, humidifying the temperature inspired air are done by the functional unit of nose named as the nasal cavity and the paranasal sinuses. 3
Lesions of the nasal cavity are quite prevalent in today’s life. Most common causes of these lesions are allergic, antigenic and obstructive. Sinonasal area is exposed to various infective agents, chemicals, antigens, mechanical, and other influences. Early detection and prompt treatment is required to eliminate the lesion. Histhopathology forms the basis of accurate diagnosis. The variation in the histopathological types and grades of the lesions, particularly malignancies has led to urgency in studying the clinical and pathological aspects. Understanding the exact nature of the lesion will help in strengthening the diagnosis and put an end to the confusions.4 This proves beneficial as the ENT out-patient department frequently receives cases of sino-nasal mass enlargement. 5
The incidence of sino-nasal masses is 1-4% in the total population. 6 Nasal polyps are a common cause of nasal obstruction in adults with 4% prevalence in the general population. 7 It has been found that the nose and paranasal sinuses account for less than 1% of all the malignant tumours and less than 3% of head and neck region malignancies. However the effect of the malignancies is crucial and it becomes vital to differentiate the range of non neoplastic lesions in this region and neoplastic lesions to understand the different treatment modality to prevent the financial and emotional burden on patient. 8
The presenting features, symptoms and advanced imaging technique might help in reaching to presumptive diagnosis but that’s not enough. Histopathological examination remains a mainstay of final definitive diagnosis for such lesions. 9
This study aims to examine the occurrence of various lesions in nasal cavity and paranasal sinuses, to determine the age, sex and site wise incidence of different benign and malignant lesions of nasal cavity and paranasal sinuses and to correlate the clinical and histopathological findings.
Materials and Methods
A descriptive study was conducted the Department of Pathology at Tertiary Healthcare Centre after getting approval of the Institutional Ethical committee and was approved by MUHS Nashik vide their list of approved title of dissertation for academic year 2017-2018. All patients with relevant clinical details irrespective of their age and gender attending the ENT OPD at a tertiary care Hospital, during a period of 2 years.
All patients with clinically diagnosed nasal and paranasal sinus lesions attending the out-patient department of ENT undergoing surgery were considered. However the patients who refused to give consent and samples that were poorly preserved in formalin were excluded.
Socio-demographic details including name, age, gender, presenting complaints, duration of complaints, general examination, local examination site and other characteristics of nasal and paranasal sinuses lesions of the subjects were considered. All this data including and radiological investigations of each patient was retrieved from the records and was mentioned in a prescribed proforma. This was noted whenever the data was possible and available.
Nasal and paranasal sinuses of the specimens in the pathology department of the designated health care centre were grossly examined. After gross examination, tissue was processed routinely by fixing specimen in 10% formalin followed by paraffin embedding. Tissue sections of 4-5 microns thickness were cut on microtome. The tissue sections were then studied in details by staining with haematoxylin and eosin stains.
Fixation for light microscopy was done for all the specimens using buffered neutral formalin for a period of 12-24 hours. Ten percent formalin, absolute alcohol, xylol, Harris haematoxylin solution, Eosin, 1% acid alcohol, DPX (Diestrene Polysterene Xylene) mounting medium and paraffin wax were the routine chemicals used in microbiological fixation. Armamentarium used for the same involved, scalpel and scissors, forceps, cassettes, L mould, rotator microscope, slides and cover slips, gloves, gauze pieces and measuring scale.
Fixation was done using 10% of formalin composed of 40% formalin (100ml), water (900ml), sodium di-hydrogen, phosphate, monophosphate (4 gm) and sodium phosphate, dibasic, anhydrous (6.5gm). Dehydration was done by three changes of graded alcohol and one change of acetone. Clearing was done using xylene. Paraffin impregnation was done twice at 60 degree Celsius. Labelled and blocks were made after trimming excess paraffin that was embedded in paraffin wax. Sections were then cut at a microtome setting of 4 microns. The sections were floated on a water bath at 600C temperature. Sections were mounted on a slide using very thin layer of glycerol egg albumin as an adhesive.
Staining technique for light microscopy was done for each block. Each block was routinely stained with (Harris haematoxylin and Eosin stain) H and E to arrive at a diagnosis. Hematoxylin crystals (5 gm), absolute alcohol (50ml), ammonium or potash alum (100 gm), distilled water (1000 ml), red mercuric oxide (2.5 gm), glacial acetic acid (40 ml) were the reagents used. H and E staining done by the technique described. Firstly deparaffinising with xylene for 5 to 10 minutes and placing the specimen in absolute ethyl alcohol, 95% of ethyl alcohol, washing with running tap water and placing it in Harris hematoxylin for 5 minutes each. Secondly, washing it with water and differentiate with 1% hydrochloric acid alcohol-ethyl alcohol, blueing with running tap water for 5 minutes then staining with aqueous 2% eosin for 1 minute, rinsing in water and 80 to 90% alcohol briefly. The specimen was then mounted in DPX after rinsing with absolute alcohol and xylene clearance twice.
The sections were then examined under the light microscope, the lesions were diagnosed as benign, malignant, and classified according to the recent WHO classification. Special stains including immunohistochemical stains were applied whenever required.
Results
3800 specimens were received in the Department of Pathology during the 2-year study period from June 2017 to June 2019. Among the total specimens, number of nasal and paranasal sinuses specimens received was 104 (2.73%). These specimens of nasal and paranasal sinuses lesions were examined and the histopathological features were classified as non-neoplastic and neoplastic (benign and malignant).
82 cases (78.84%) were found to be non-neoplastic and 22 cases (21.16%) were reported as neoplastic lesions. Majority with 24 cases (20.92%) belonged to 21-30 years age group followed by 31-40 years age group with 23 cases (20.84%) and least common age group affected was 0-10 years with 2 cases (1.94%). Cases belonged to the age ranging from 6 years to 76 years. The gender-wise comparison between nasal and paranasal lesions exhibited that the lesions were more common in male population 55 (53.39%) cases and the remaining were females.
The nasal and paranasal sinuses were identified initially by clinical representation of the lesions. It was observed that the most common clinical feature was nasal obstruction seen in 97 cases (93.26%). The clinical presentations of the lesions have been represented in the [Table 1].
The site-wise distribution was observed and it was observed that most common site for lesions was nasal cavity 82 cases (78.84%), whereas 22 cases (21.16%) were present in the paranasal sinuses and the occurrence of lesions when the laterality was observed showed that 32 cases (30.76%) were bilateral, 34 cases (32.69%) were arising from the left side and 38 cases (36.55%) were arising from the right side of nasal cavity.
Polyps were found to be the most common lesions for non-neoplastic lesions. Frequency and percentages of percentage of non-neoplastic lesions, benign neoplasms and malignant neoplasms are represented in [Table 2].
Age-wise distribution for non-neoplastic lesions represented that the most common non-neoplastic nasal and paranasal lesion was inflammatory nasal polyp with 66 (80.48%) cases followed by allergic nasal polyp with 8 (9.75%) cases and fungal infections like; Rhinosporidiosis, Mucormycosis and Aspergillosis consisted of 1 (1.21%) case each. Most of the inflammatory nasal polyps were seen in the age group of 31-40 years. Fungal infections were mainly seen in age groups 11 to 30 years and 61-70 years age group. Age-wise distribution of the neoplastic and non-neoplastic lesions of nasal is depicted in [Table 3]. Rhinosporidiosis is depicted in [Figure 1].
Table 1
Clinical presentation of nasal and paranasal sinuses lesions
Table 2
Lesion wise categorical distribution
|
Lesion |
|
Number of cases |
Percentage |
|
Non-neoplastic |
Polyps |
74 |
71.84% |
|
Others |
8 |
7.76% |
|
|
Neoplastic |
Benign |
16 |
14.56% |
|
Malignant |
6 |
5.84% |
|
|
Total |
|
104 |
100% |
Table 3
Age wise distribution of nasal and paranasal sinuses lesions
Table 4
Distribution of histopathological feature of nasal and paranasal sinuses
Table 5
Sex wise distribution of lesions in nasal cavity and paranasal sinuses
[Table 4] shows histopathological distribution of the lesions of nasal and paranasal sinuses. It clearly describes the histological types of non-neoplastic, benign and malignant lesions and their prevalence in the study.
Gross appearance of inflammatory polyp is shown in [Figure 2]
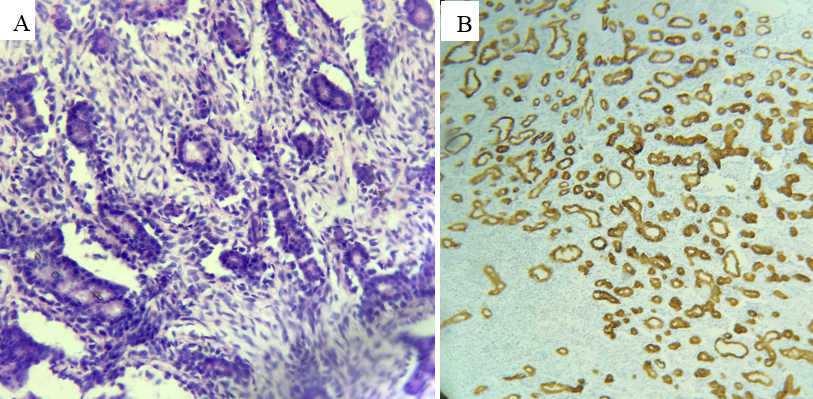
Neoplastic lesions were further classified as benign and malignant. Of 104 specimens, nasal neoplasms were reported in 22 cases out of which 16 cases (14.56%) were benign. In these neoplasms, the most common benign neoplasm was hemangioma (microscopy depicted in [Figure 3]) reported in 8 (50%) followed by three (18.75%) cases of inverted papilloma [Figure 4]. Majority of the benign lesions were found in 41-50 years of age. However hemangioma was most common among the age group of 11 to 60 years.
6 cases (5.84%) were found to be malignant. The most common malignant neoplasm was squamous cell carcinoma reported in 3 (50%) of cases and 1 (16.67%) case each of Acinar cell Carcinoma, Primitive Neuroectodermal Tumour and Olfactory Neuroblastoma [Figure 5]. Malignant neoplasms were majorly reported after 5th decade of life.
This distribution was also studied by gender and it was found among Non-neoplastic Lesions that of the 66 total cases of inflammatory polyps, 60% (39 cases) were males and 40% (27 cases) were females.
Out of 08 cases of allergic nasal polyps, 6 cases (75%) were females and 2 (25%) cases were males, 4 cases of rhinosporidiosis, were seen equally in males and females 2 (50%) cases each. Mucormycosis [Figure 6], aspergillosis showed 1 case each in females. Rhinoscleroma and nasolabial cyst were reported in 1 case each in males. Benign neoplastic lesions showed a female predominance. Gender-wise distribution among Benign and Malignant neoplasms is represented in [Table 5]. Immunohistochemistry was done for diagnosing Pleomorphic Adenoma as Benign Mixed Tumour shown in [7Figure 7a,b] was given on light microscopy. The tumour showed glands immunopositive for CK 14/ CK 19 and myoepithelial cells immunopositive for p63/ Smooth muscle actin. Immunohistochemistry was also helpful in difficult diagnosis of Malignant Small Round Cell Tumour which showed membranous immunopositivity for CD99 and FLI1 which gave a diagnosis of Primitive Neuroectodermal Tumour.
Clinico-histopathological diagnosis
In the study, out of 80 cases that were clinically diagnosed inflammatory nasal polyps, 73 (91.25%) cases were reported as inflammatory nasal polyps on histopathology. Similarly seven out of eight cases of hemangioma were diagnosed histopathologically. Inverted papilloma was clinically diagnosed in three cases, of which two (66.66%) cases were reported as inverted papilloma histopathologically. Four cases were clinically diagnosed as malignant were proved malignant on histopathology. Ninety-two cases of the total clinically diagnosed 104 cases were confirmed through histopathological examination. The similarity in clinico-histopathological was found to be 88.46%.
Immunohistochemistry of Primitive Neuroectodermal Tumour is shown in [Figure 8].
In the present study, the most common complaint was nasal obstruction seen in 97 cases (93.26%) followed by rhinorrhoea seen in 73 (70.19%). Least common complaint was facial swelling seen in 24 cases (23%).Table 1
In present study, polyps were the most common lesions accounting for 74 (71.84%) cases in non-neoplastic lesions. The percentage of benign neoplasms put of 104 cases were 16 cases (14.56%) and malignant neoplasms were 6(5.84%).Table 2
In present study, as mentioned in above Table out of 104 cases, majority of cases belonged to 21-30 years age group(20.92%) followed by 31-40 years age group(20.84%) and least common age group affected was 0-10 years with (1.94%).Table 3
Youngest case was of 6 years old girl and oldest case was of 76 years old female
In our study, nasal and paranasal lesions were more common in males accounting for 55 (53.39%) cases and 48 (46.61%) in females.Table 5
Figure 1
Rhinosporidiosis; 100X microscopy showing thick walled sporangia containing daughter spores.
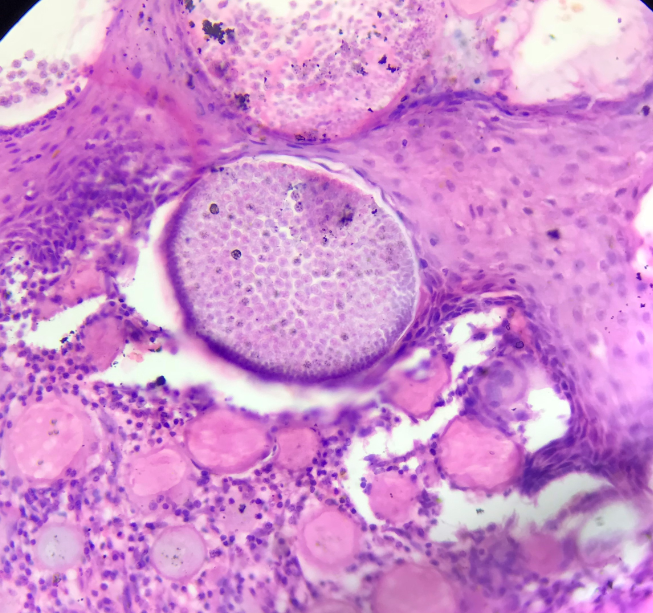
Figure 2
Inflammatory polyp,Gross appearance of inflammatory nasal polyp- white, glistening, polypoidal, soft in consistency

Figure 3
Hemangioma;40X microscopy showing stratified squamous epithelium below which are vascular proliferating capillaries arranged in lobules or clusters
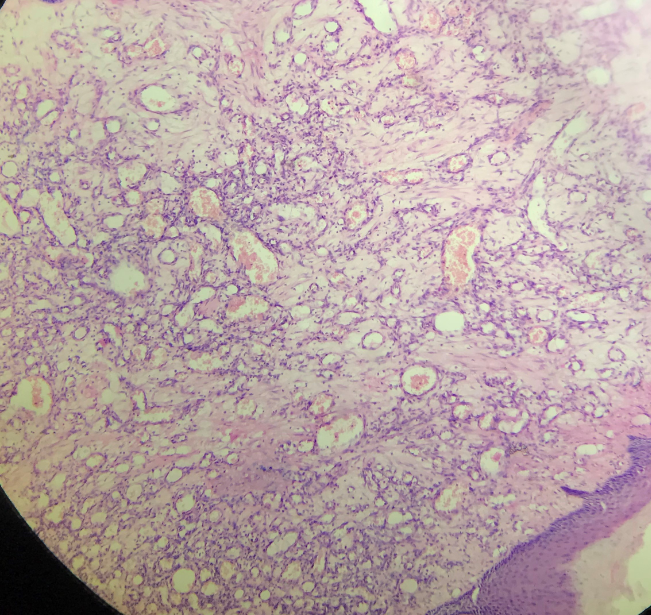
Figure 4
Inverted papilloma;40X Multiple inversions of the surface epithelium into the underlying stroma composed of squamous cells lined by a basement membrane. Stroma is loose with loss of seromucinous glands.
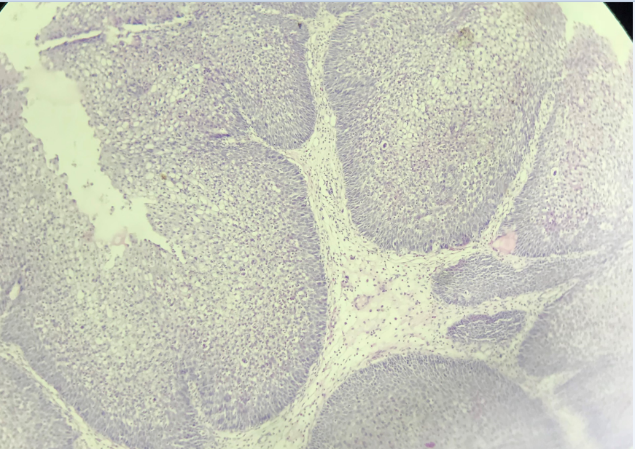
Figure 5
Olfactory neuroblastoma;10X microscopy showing lobules of ‘primitive’ neuroblastoma cells separated by vascularized fibrous stroma.
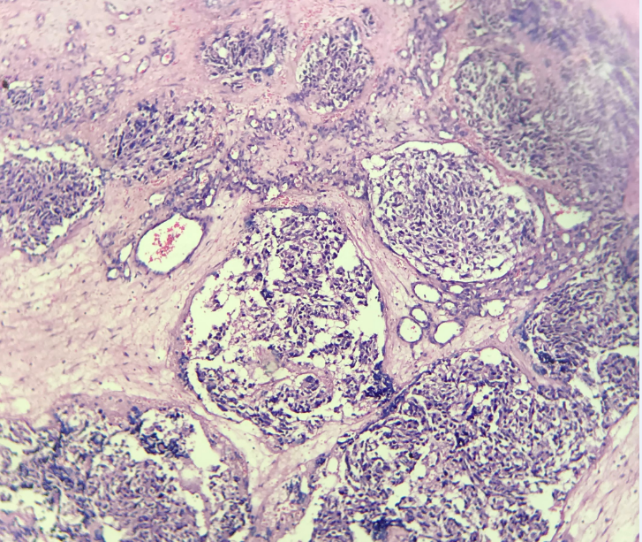
Figure 6
Mucormycosis; 40X power microscopy showing large fungal hyphae, which are non-septate and have a ribbon like appearece, with budding and dichotomous branching.
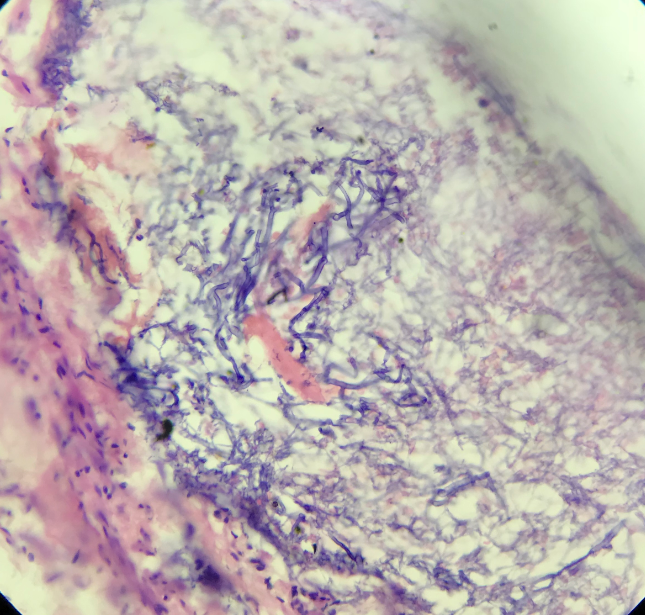
Figure 7
A: Pleomorphic adenoma; 40X microscopy showing epithelial predominance than stromal. The epithelial cells are cuboidal, small, oval shaped arranged in small acinous structures. The solid component shows spindle shaped cells along with myxoid areas; B: Pleomorphic adenoma; Immunohistochemistry showing glands positivity for CK19.
Discussion
Wide arrays of non-neoplastic and neoplastic conditions involve the nasal cavity (NC) and paranasal sinuses (PNS), and these are very common lesions encountered in clinical practice. The presenting features, symptoms and advanced imaging technique help to reach a presumptive diagnosis but histopathological examination remains the mainstay of final definitive diagnosis. It becomes impossible to differentiate non-neoplastic and neoplastic lesions clinically and diagnosed as nasal polyp.
This study was conducted with the objective to study clinical features and histopathological finding of nasal cavity and paranasal sinuses lesions according to age, gender and site during a period of 2 years. During this period, total 104 specimens of nasal cavity and paranasal sinus lesions were diagnosed and analysed in the Department of Pathology of the study institute to achieve the above mentioned objectives.
The study found 78.5% of the sinonasal lesions to be non-neoplastic and 21.5% to be neoplastic. Similar results were observed in a study by Lathi A. et al in 2011, 10 studied clinicopathological profile of sinonasal masses at rural tertiary care hospital, found 71.4% lesions as non-neoplastic and 28.6% as neoplastic. Humayun et al, 11 Garg D et al 1 observed non-neoplastic sinonasal lesions in 70%, 73.6%, 72% cases respectively while neoplastic lesions in 30%, 26.4%, 28% cases respectively. The findings were also in accordance with the study by Ghanghurde S et al 8 and Dasgupta et al. 12
Among the cases studied, 20.92% of the subjects mainly belonged to the age group of 21-30 years with age range from 6 years to 76 years. A study by Lathi A et al 10 exhibited similar percentages reported maximum sinonasal lesions in 11-20 years and 31-40 years (20.5%). Post analysis, maximum numbers of non-neoplastic lesions were seen in the age range of 21-40 years. Benign neoplastic lesions were common in 41-60 years while malignant neoplastic lesions were frequent after 30 years of life. Lathi A et al, 10 Humayun et al 11 and Nayak M et al 9 reported similar findings.
55 males had lesions of nasal cavity and paranasal sinuses and the male to female ratio was found as 1.2:1. Various studies like Sharma R et al, 6 Lathi A et al, 10 Maheshwari A et al, 5 also noted male preponderance in lesions of nasal cavity and paranasal sinuses with male to female ratio 1.3:1, 1.5:1 and 1.8:1 respectively.
Maximum number of the cases 72 (69.24%) showed unilateral presentation. Our findings were similar to result of Sharma R et al 6 (68%) and (67.31%), Maheshwari A et al 5 (56.25%).
Nasal cavity was the commonest site 82 (78.84%) for these lesions. Shah S et al3 also showed higher number of lesions in the nasal cavity with 69%.
97 cases presented nasal obstruction as the chief complaint and results of various other studies reported the same. Humayun et al, 11 Lathi A et al, 10 Maheshwari et al 5 reported nasal obstruction as the most common complaint with 47 (94%) cases, 108 (97.3%), 71 (88.75%), 37 (88%) cases respectively. Second most common complaint was rhinorrhoea with 73 (70.19%) cases which was consistent with Maheshwari et al, 5 Bist et al 13 with 58 (72.5%) and 76 (69.09%) cases.
The maximum numbers of non-neoplastic lesions were seen in 2nd and 3rd decade. Studies by Nayak M et al, 9 Lathi A et al,10 Garg D et al (2014), 1 reported their incidence in the 3rd and 4th decade. Non- neoplastic lesions were more common in male population (54.87%). This was consisitent with few studies and inconsistent in a study by Parajuli et al. 7
The most common nasal lesion was the simple nasal polyp and was consistent with all other comparable studies. The second most common nonneoplastic was rhinosporidiosis and was comparable to the cases which were comparable to a study done by Parajuli et al 7 in the year 2013. Fungal infections were found less prevalent in the studies by; Maheshwari A et al, 5 Mane P et al and Garg D et al. 1 The study also showed that the fungal infections are most common among females however it was more common among males in studies by different authors.
Rhinoscleroma was the least reported 1 (1.21%) and was much higher in the study by Lathi A et al with incidence of 10%.
Among benign lesions, incidence of benign lesions was more common in males with 10 (62.5%) cases than females with 6(37.5%) cases. This finding was comparable with Lathi A et al, Mane P et al, 2 with 12 (63.15%), 13(72.22%), and 12 (80%) cases respectively. Parajuli S et al 7 reported a higher incidence of benign lesions in females with 11 (57.90%).
Most common age group affected with benign lesions was 41-60 years.
Hemangioma was the most common benign lesion comprising of 8 (7.76%) cases which was comparable to Lathi A et al, 10 Maheshwari A et al 5 with 9 (8.03%) cases and 7 (8.75%) cases respectively. The incidence of hemangioma was maximum in the 2nd, 3rd, 4th decade comparable with Garg D et al. 1 Incidence of schwannoma, pleomorphic adenoma, fibroma, neurofibroma, angiofibroma was very less and comparable to other studies. Hemangioma was seen equally in both sexes (M: F=1:1), however, Ghanghurde S et al 8 in 2017 reported a higher incidence of hemangioma in males than females.
Among malignant neoplasms, squamous cell carcinoma was the most common malignant neoplasm comprising of 3 (2.91%) cases which was in accordance with Lathi A et al, 10 Maheshwari A et al, 5 Garg D et al 1. Sixty-six percent of the males exhibited malignant lesions in this study. Studies by Humayun et al, 11 Parajuli S et al 7, Lathi A et al 10 reported a higher incidence in males with 66.67%, 60% and 76.92% respectively. Mane P et al 2 however reported a higher prevalence in females.
One case of Acinar cell Carcinoma was reported in the age of 76 years and one case of Primitive Neuroectodermal Tumour. Immunohistochemistry was done in this case which was focally positive for CD 99, and vimentin. Garg D et al in 2014 also reported one case of PNET suggesting its rarity.
Similarity in the diagnosis by clinical and histopathological was present in 88.46% cases. Sharma R et al (84%), 6 Bist et al (96.37%), 13 Gupta et al (96%) 14 and Kale et al 15 studied 344 cases and found clinico- histopathological similarity in 99.7% cases diagnosed.
Conclusion
The nasal and paranasal lesions most commonly affected the age group of 21-40 years with male preponderance seen in 53.39% of cases. Inflammatory nasal polyp is the most common non-neoplastic condition affecting both males and females, hemangioma was the commonest benign neoplasm and squamous cell carcinoma is the commonest malignant neoplasm.
We concluded that complete clinical, radiological and histopathological correlation helps us to categorize these sinonasal lesions into various non-neoplastic and neoplastic types. But final histopathological examination provides a confirmatory diagnosis, as a significant number of cases may be missed on clinical evaluation alone.
The presenting clinical features of non-neoplastic and neoplastic nasal and paranasal sinuses lesions may be indistinguishable from each other leading to delay in proper diagnosis and treatment. Histopathological examination is a reliable, cost effective diagnostic tool for accurate diagnosis and management of various lesions of nasal cavity and paranasal sinuses, as a significant number of cases may be missed on clinical evaluation alone.

