Introduction
Primary Squamous cell carcinoma of the renal pelvis is rare and accounts to only 0.5- 0.8 % of malignant renal tumours. They are highly aggressive in nature and carries poor prognosis.1
Chronic irritation, inflammation and infection induce the pathogenesis of this malignancy Urothelium, histologically does not have the Squamous cells, hence it is assumed that due to chronic irritation, which can be due to pelvic stone, as in our case or any inflammation or infection, leads to dedifferentiation, metaplasia, dysplasia and finally leading to Squamous cell carcinoma.2
Case Report
Here, we report a case of a 53 year old male patient, presented to our Urology Department with left flank pain since one month. He was taking regular analgesic for the same. On Per abdomen examination no abnormality was detected.
On radiological investigation, his CT revealed atrophic shrunken left kidney measuring 7.9x5.2cms showing significant parenchymal thinning and complete loss of corticomedullary differentiation. The left renal outline is distorted with dilated calyceal system. Ill- defined heterogenous mass in the inter-polar region. Few small reactive peri-renal lymph nodes are seen. A left upper ureteric calculus is seen measuring 7.5 mm with significant left renal hydronephrosis. Right Kidney shows compensatory hypertrophy. Clinically, it was diagnosed as Xanthogranulomatous Pyelonephritis.
Table 1
Significant laboratory markers
|
Creatinine |
0.91 mg/dl |
|
Sodium |
135mEq/L |
|
Potasium |
4.87 m Eq/L |
|
Albumin |
5g/dL |
|
HbA1c |
9.4 % |
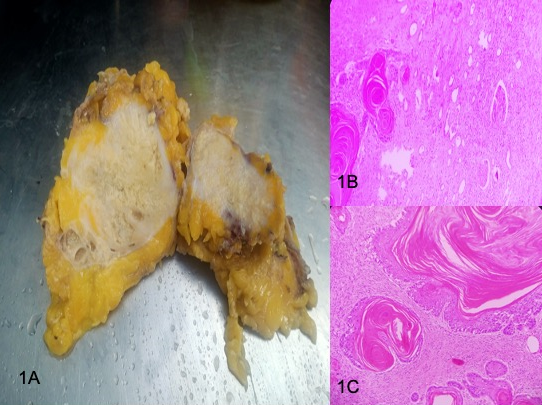
On histopathology, grossly the radical nephrectomy specimen measuring 10.5x5.5x3.5 cm & weighing 150 gm. Attached ureter mg 5.0x0.5 cm. External surface is irregular & bosselated. On Cut surface renal architecture is effaced by necrotic mass measuring 9.5x5.0x3.0 cm involving pelvic ureter and most of renal parenchyma. Adrenal gland mg 5x1x0.5 cm and is unremarkable.[Figure 1 A]
Hematoxylin and eosin stained tissue revealed characteristic feature such as keratin pearls and intracellular bridges seen, rendering the diagnosis of well-differentiated keratinising squmaous cell carcinoma seen infiltrating the kidney parenchyma and perinephric-pelvic fat with 40 % tumour necrosis. All the resected ureteral, deep soft tissue and renal hilar soft tissue margins were uninvolved by invasive carcinoma and showed no features of in- situ carcinoma. 5 lymph nodes were retrieved and showed reactive lymphoid hyperplasia additional pathologic findings associated were Inflammation/regenerative changes, Keratinizing Squamous Dysplasia and Chronic Pyelonephritis.[Figure 1B,C]
Figure 1
A: Gross photograph of kidney, showing complete effacement of renal architecture by necrotic material; B: Microphotograph showing keratin pearls invading the renal parenchyma (H and E stain X100); C: Microphotograph showing features of well- differentiated Squamous cell carcinoma (H and E stain X 400).
Discussion
SCC in the kidney is very unusual and is known to arise from collecting system.
There is a female predominance and the most common age group of presentation is 50–70 years. For primary renal parenchymal SCC, renal pelvis should be histologically normal. Histopathologically, squamous components in SCC of kidney are similar to other SCCs and consist of features of keratin pearls, intercellular bridges, and keratotic cellular debris. If the urothelial dysplastic element is identified along with urothelial carcinoma in situ, the tumour should be classified as primary urothelial carcinoma with Squamous differentiation. In order to call it as primary SCC of renal parenchyma, metastasis from other sources should be ruled out and histopathology of the renal pelvis should be normal despite other findings. There may be possibility of an occult primary SCC somewhere in the body. In the present case, etiological factor was obstructive uropathy due to renal calculi which has triggered the event of malignancy. The radiologic differential diagnosis includes primary and secondary renal neoplasms and xanthogranulomatous pyelonephritis (XGP) associated with renal calculi. XGP is commonly associated with lithiasis however, rarely causes keratinizing squamous metaplasia and its manifestations closely mimic renal neoplasm, leading to misdiagnosis of malignancy.3, 4
Imbriaco et al.,5reported renal SCC within a horseshoe kidney associated with renal stones with non-specific CT and MRI findings. The non-specific clinical and radiologic features in renal SCC may cause diagnostic confusion and histopathology is needed for confirmation.
Radical Nephrectomy is the mainstay of treatment in SCC of renal pelvis. Renal SCC usually presents at an advanced stage-pT3 or higher there is no standard guideline regarding treatment of primary renal parenchymal SCC. The present case was treated with radical nephrectomy. According to previous data, the incidence, etiopathogenesis, clinical course, management, and prognosis of primary renal parenchymal SCC is inconclusive. It needs a large number of case studies with proper evaluation and management.
The prognosis is dismal with a 5-year survival rate of less than 10%.
Conclusion
Primary renal SCCs are rare tumors and show a strong association with renal stones. Image features on conventional radiographic studies are non-specific. SCC should be suspected in any patient presenting with renal pelvis mass and history of renal calculi. CT and MRI play a crucial role in diagnosis and staging of these tumors, though histology is always remains confirmatory and diagnostic.
