- Visibility 328 Views
- Downloads 66 Downloads
- Permissions
- DOI 10.18231/j.jdpo.2021.048
-
CrossMark
- Citation
Primary umbilical endometriosis – A rare presentation of cutaneous endometriosis
Abstract
Primary umbilical endometriosis is a rare condition with an overall incidence of around 0.5% to 1% among all the endometriosis cases, but at times it poses a diagnostic dilemma. In our institution we encountered a case of primary umbilical endometriosis presented to multiple surgical speciality departments. A prompt clinical examination with surgical biopsy was the key tool which lead to the diagnosis and providing a complete cure for the patient. Pelvic endometriosis affects 5-10% of women in the child bearing age group. The most pronounced symptoms are dyspareunia, pelvic pain, and infertility. Clinical presentations of umbilical endometriosis are as a nodule with or without associated umbilical pain and bleeding. This patient was given primary hormonal therapy and later underwent a biopsy which paved way for an accurate diagnosis of primary umbilical endometriosis. In this case of umbilical swelling, conditions like a benign nevus, lipoma, abscess, cyst, hernia, as well as metastatic deposit from a systemic malignancy were considered in the clinical differential diagnosis. However surgical excision helped us arrive at a definitive diagnosis and cure for the patient.
Introduction
Endometriosis is a frequent pathology seen in 5-10% of women in childbearing ageand commonly involves the lower pelvis. It is also known as Villar’s Nodule named after the person who first described it, Villar in the year 1886. Endometriosis is defined as the presence of endometrial glands and stroma outside the uterus and the cause of which is poorly explained. Various studies and researchers has proposed the possible cause as ectopic implantation of endometrial tissue following retrograde menstruation as the cause of this condition.[1] The prevalence of endometriosis is estimated to range between 4% in asymptomatic women and 50% in women with dysmenorrhea.[2] A review of literature also suggests that the prevalence of endometriosis increases with age. [3], [4]
Common locations of endometriosis are the pelvic organs, mostly ovaries, uterosacral ligaments, rectum and the bladder. However cutaneous endometriosis is a rare entity of which the incidence of primary umbilical endometriosis is about 0.5-1% among all the women with extra gonadal endometriosis.[5] A scar endometriosis can occur in a sub-umbilical incision scar commonly due to a cesarean section and primary umbilical endometriosis has to be differentiated from this entity.[6] According to the literature, a total of only 109 cases of umbilical endometriosis has been reported.[7] The presentation of endometriosis to the general surgeons is rare, and with atypical symptoms, it poses diagnostic difficulties.[8] The umbilicus is one of the less common sites for the localization of the ectopic endometrial tissue. Various theories with regards to the pathogenesis of endometriosis have been suggested, none of which can unequivocally account for the endometriosis in all the various locations in which it has been reported.
Case Report
A 37 year old multiparous women, presented to OBG OPD with complaints of pain and bleeding from umbilicus during her menstruation. She gives history of noticing a nodule over the umbilicus associated with pain during her menstrual cycle, without any associated bleeding from the site, for the past 6 years,. She had consulted at an outside hospital in the year 2016 for the same. After routine investigations, she underwent a biopsy evaluation of the umbilical nodule on 27/4/2016. A diagnosis of Endometriotic nodule was suggested. Two years after the biopsy, she started to notice bleeding from the umbilicus during menstruation associated with pain. She then consulted at the OBG department of our hospital, in august 2018. On physical examination there was a dark discolouration and tenderness over umbilicus at the time of presentation. She was given a single dose of Medroxyprogesterone 150mg injection and was adviced a repeat the same after two weeks. Later, after two months, she again presented with complaints of pain and bleeding through the umbilicus and presented to the Surgery OPD. Her medical history was unremarkable. She did not give any history of symptoms of pelvic endometriosis such as dysmenorrhea, abdominal pain or dyspareunia. Her LMP (last menstrual period) was on 25/07/2018. She was not on any other oral contraceptives except for the two dose of Medroxyprogesterone which was given two months prior. She was investigated as per the routine. USG abdomen revealed a normal study except for a seedling fibroid in the fundus of uterus. A provisional diagnosis of Primary umbilical endometriosis was made and she was posted for surgical excision of the umbilical nodule. There was no history of Diabetes mellitus, Hypertension, Tuberculosis, Bronchial asthma or Thyroid disorders for her. No history of any drug intake or drug allergies in the past.
She was evaluated in the surgery department. Physical examination revealed a single swelling of size 2 x 1 cm arising from the umbilicus. Surgical removal of the nodule was done. Post- operative period was uneventful.
Pathology evaluation
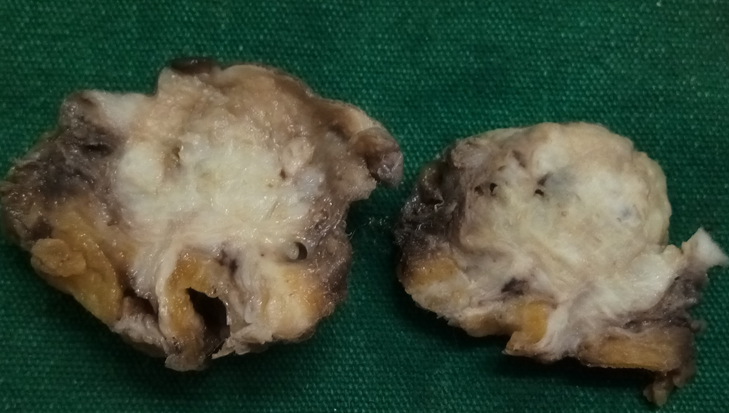
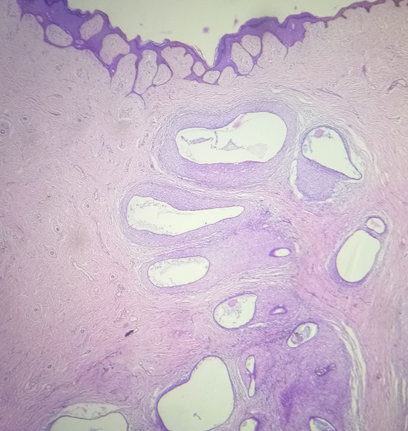
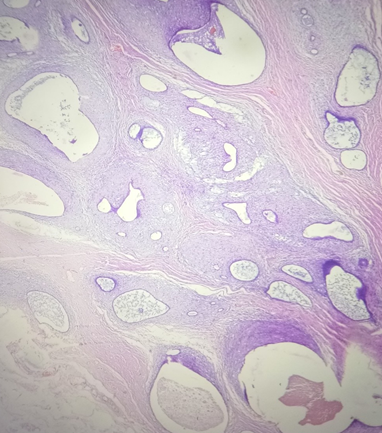
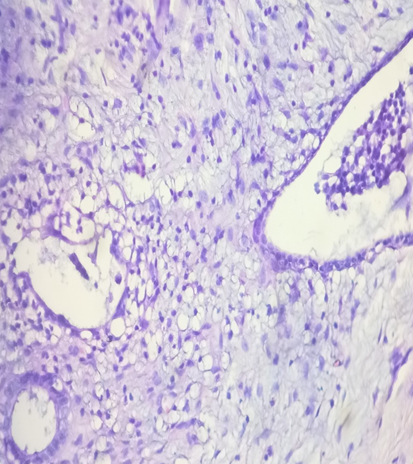
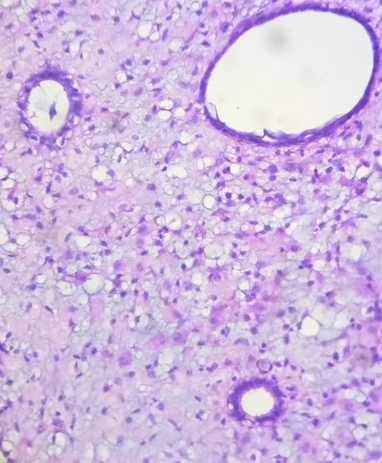
In the department of Pathology, we received the sample of excised umbilical nodule. Grossly it was a skin attached soft tissue fragment measuring 4x3.5x2cm. A raised grey brown area was noted on the surface of skin measuring about 1.5cm in diameter. Cross section of the specimen revealed grey brown areas with tiny hemorrhagic spots. [[Figure 1], [Figure 2]] Histopathological evaluation showed intact epidermis. The dermis showed multiple cystically dilated glands with endometrial type of columnar cell lining. The glands had amphophilic secretions in its lumen and hemosiderin laden macrophages admixed amongst the epithelial cells. The stroma surrounding the glands were exhibiting decidualisation and myxoid changes. Scattered inflammatory cell infiltrates were also noted in the stroma. A histopathological diagnosis of Cutaneous Endometriosis was made. [[Figure 3], [Figure 4]]
Discussion
Pelvic endometriosis may present with symptoms like dyspareunia, pelvic pain, and infertility.[9] The other symptoms may include diarrhea, constipation and abdominal bloating particularly during menstrual period, heavy or irregular bleeding and fatigue.[10] The clinical presentations of umbilical endometriosis can be as pigmented nodule or umbilical weeping, especially cyclical bleeding and cyclical pain.[11] In our case the patient was having cyclical pain in the umbilicus during menstruation but without any bleeding manifestations from the umbilicus for many years. A surgical intervention was done from umbilical nodule for biopsy evaluation, following which she developed bleeding from that site during her menstruation. No other cause could be attributed to the bleeding manifestation as she had not underwent any other surgeries in the past and both her children were born out of normal vaginal delivery. In this case the stroma surrounding the glands showed changes of decidualisation. This may be attributed to hormonal therapy which she received before the surgical resection. A Primary umbilical endometriosis is a rare occurrence but while considering umbilical disorders in women with no typical symptoms of pelvic endometriosis, it should come in the differential diagnosis. The umbilicus is a preferred spot for cutaneous endometriosis; however, only 4 cases of primary umbilical endometriosis surgically confirmed not to have endometriotic lesions in the abdominal cavity have been reported in previous literature.[12], [13], [14] As in our case the ultrasound evaluation of abdomen and pelvis did not reveal any lesions suggesting adenomyosis of uterus or endometriosis in the gonads and fallopian tubes. With regard to this information our case of primary umbilical endometriosis without any other foci in pelvis or uterus, stands out as a rare entity. The theory of lymphatic or hematogenous spread is favored with primary umbilical endometriosis, although the etiology of umbilical endometriosis is not completely understood.
Most of the endometrial deposits are found in the pelvic region, ovaries, fallopian tubes, cervix, pelvic peritoneum, uterosacral ligaments, pouch of Douglas and the rectovaginal septum. There may be rare occurrence in extragonadal and extra pelvic locations. These include most of the body cavities, as well as organs like lung, gallbladder, intestine, kidney, brain, extremities, perineum, and abdominal wall. Extra pelvic endometriosis may occur in up to 12 % of the women with endometriosis. There are medical and surgical treatment modalities in umbilical endometriosis. In treating pelvic pain, both medical and surgical treatments are effective.[15] Pre- operative hormone therapy may be used in patients with large mass of umbilical endometriosis, to reduce the size.[16] In our case the patient was given hormonal therapy with parenteral medroxyprogesterone injections, followed by a surgical excision. A post excision defect of umbilicus can mostly be repaired directly by using a skin flap, without much disfigurement.[17] Hormonal therapy may be considered when there is a coexistent pelvic endometriosis.[18] The risk of malignant transformation from umbilical endometriosis is very low. Some rare cases had undergone malignant transformation into endometrial carcinomas. The possibility of a coexisting genital-pelvic endometriosis must be investigated for.
The development of umbilical endometriomas can occur following laparoscopic surgical procedures involving umbilicus. Several theories have been proposed with regard to the pathogenesis of cutaneous/umbilical endometriosis, with coelomic metaplasia being the most favoured one. Also the umbilicus may act as a physiological scar where the remnants of endometrial tissue may be seen which can pave way for the development of spontaneous umbilical endometriosis. In certain scenarios like malignant melanoma presenting as an umbilical nodule or a “sister Mary Joseph nodule”— which may be an umbilical manifestation of an intra-abdominal malignancy there can arise a diagnostic dilemma. In case of an umbilical swelling, conditions like a benign nevus, lipoma, abscess, cyst, or hernia, as well as metastatic deposit from a systemic malignancy, should be considered in the clinical differential diagnosis. However a biopsy with a thorough histopathological examination will be helpful in arriving at a definitive diagnosis in such situations.
Conclusion
Primary umbilical endometriosis is a rare condition with an overall incidence of around 0.5% to 1% among all the endometriosis cases, but at times it poses a diagnostic dilemma. Hence, a histopathological examination is necessary for confirmation of diagnosis. Treatment modalities include hormonal therapy and surgical excision. A preoperative hormone therapy may help in reducing the size of the umbilical lesion but may not provide a cure for the condition. However the treatment of choice is always a complete surgical resection having an extremely low recurrence rate.
Conflict of Interest
There is no potential conflict of interests related to the exclusive nature of this paper.
Source of Funding
No financial support was received for the work on this manuscript.
References
- Hooghe TM, Hill JA. Endometriosis. Novak's Gynecology. 17th Edn.. 2007;29. [Google Scholar]
- Cramer DW, Missmer SA. The epidemiology of endometriosis. Ann N Y Acad Sci. 2002;955:11-22. [Google Scholar] [Crossref]
- Fritzer N, Haas D, Oppelt P, Renner S, Hornung D, Wolfler M. More than just bad sex: sexual dysfunction and distress in patients with endometriosis. Eur J Obstet Gynecol Reprod Biol. 2013;169(2):392-6. [Google Scholar]
- Tavasoli F, Hafizi L, Aalami M. Pelvic Endometriosis in a Patient with Primary Amenorrhea. J Reprod Infertil. 2009;10(2):145-50. [Google Scholar]
- Michovitz M, Baratz M, Stavorovsky M. Endometriosis of the umbilicus. Dermatologica. 1983;167(6):326-30. [Google Scholar]
- Panicker S, Pillai N, Nagarsekar U. Villar’s Nodule: A rare presentation of external endometriosis. MJAFI. 2010;66(1):70-71. [Google Scholar] [Crossref]
- Blumenthal N. Umbilical endometriosis; a case report. SA Med J. 1989. [Google Scholar]
- Firilas A, Soi A, Max M. Abdominal incision endometriomas. Am Surg. 1994;60(4):259-61. [Google Scholar]
- Chatzikokkinou P, Thorfinn J, Angelidis IK, Papa G, Trevisan G. Spontaneous endometriosis in an umbilical skin lesion. Acta Dermatoven APA. 2009;18(3):126-30. [Google Scholar]
- D’hooghe TM, Hill JA, JB, EA, PH. Endometriosis. Novak’s Gynaecology. 13th Edn.. 2002. [Google Scholar]
- Frischknecht F, Raio L, Fleischmann A, Dreher E, Luscher KP, Mueller MD. Umbilical endometriosis. Surg Endosc. 2004;18(2). [Google Scholar] [Crossref]
- Kimball KJ, Gerten KA, Conner MG, Richter HE. Diffuse endometritis in the setting of umbilical endometriosis:a case report. J Reprod Med. 2008;53(1):49-51. [Google Scholar]
- Fernández-Aceñero MJ, Córdova S. Cutaneous endometriosis: review of 15 cases diagnosed at a single institution. Arch Gynecol Obstet. 2011;283(5):1041-4. [Google Scholar] [Crossref]
- Dadhwal V, Gupta B, Dasgupta C, Shende U, Deka D. Primary umbilical endometriosis: a rare entity. Arch Gynecol Obstet. 2011;283(1):119-20. [Google Scholar]
- Olive DL, Pritts EA. Treatment of endometriosis. N Engl J Med. 2001;345(4):266-75. [Google Scholar] [Crossref]
- Purvis R, Tyring S. Cutaneous and subcutaneous endometriosis. J Dermatol Surg Oncol. 1994;20:693-5. [Google Scholar]
- Franco D, Medeiros J, Farias C, Franco T. Umbilical reconstruction for patients with a midline scar. Aesthetic Plast Surg. 2006;30:595-8. [Google Scholar]
- Shrestha NS, Pande S, Joshi M, Padhye SM. Primary umbilical endometriosis-A case report. NJOG. 2011;6(1):51-2. [Google Scholar]
How to Cite This Article
Vancouver
C G, K MAK. Primary umbilical endometriosis – A rare presentation of cutaneous endometriosis [Internet]. IP J Diagn Pathol Oncol. 2021 [cited 2025 Nov 07];6(3):226-230. Available from: https://doi.org/10.18231/j.jdpo.2021.048
APA
C, G., K, M. A. K. (2021). Primary umbilical endometriosis – A rare presentation of cutaneous endometriosis. IP J Diagn Pathol Oncol, 6(3), 226-230. https://doi.org/10.18231/j.jdpo.2021.048
MLA
C, Girija, K, Muhammed Aslam K. "Primary umbilical endometriosis – A rare presentation of cutaneous endometriosis." IP J Diagn Pathol Oncol, vol. 6, no. 3, 2021, pp. 226-230. https://doi.org/10.18231/j.jdpo.2021.048
Chicago
C, G., K, M. A. K.. "Primary umbilical endometriosis – A rare presentation of cutaneous endometriosis." IP J Diagn Pathol Oncol 6, no. 3 (2021): 226-230. https://doi.org/10.18231/j.jdpo.2021.048
