Introduction
In 1904, Albrecht was the first one to use the term ''hamartoma''.1, 2, 3 Hamartomas are not true neoplasm but are primary non-neoplastic malformations or inborn errors of tissue development, characterized by an abnormal mixture of native tissues of a part of the body with an excess of one or more of the cellular components. These are commonly seen in respiratory and digestive organs, such as the lungs, pancreas, and liver.4
Histologically the tongue tumors in children can be classified as solid tumors, excretory cysts, lymphovascular masses, and reactive epithelial lesions.5 Unlike true neoplasms, they do not exhibit any unchecked monoclonal tissue proliferation.
Case Report
This report describes a 5-year-old girl who presented with a sublingual swelling which was initially diagnosed as a cyst for which she underwent surgical excision. The affected person had no other medical issues. The diagnosis of hamartoma was made after histopathological analysis or examination. There have been no signs of recurrence. This report summarizes the relevant literature.
HISTORY- 5y/f presented to surgery OPD with complaints of bluish swelling under the tongue on the ventral surface for 1 year. The size of the swelling was 2x2 cm with no discharge. The diagnosis made after the initial examination was a cyst.
Investigations
The laboratory tests carried out were within the normal range.
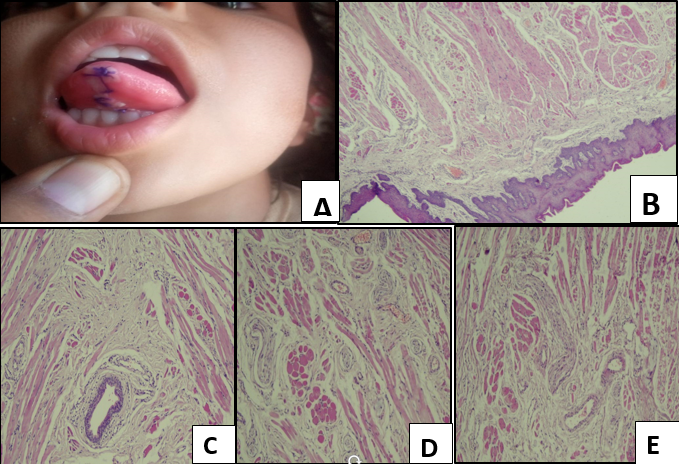
After the lab investigations, she was planned for the surgery. The excision of the swelling was done on 09/04/21. There were no complications after the operation. The swelling was sent to us for histopathological examination. The histopathological examination showed stratified squamous epithelium revealing parakeratosis, marked acanthosis, and papillomatosis. The sub-epithelial tissue comprising of haphazard arranged skeletal muscle fibers, nerve bundles, dilated and engorged vessels of variable thickness, and salivary ducts, a couple of mucinous glands.
Figure 1
Photomicrograph (A) shows post operative cyst area which was removed surgically. Photomicrograph; (B) showed stratified squamous epithelium revealing parakeratosis, marked acanthosis and papillomatosis. Photomicrograph; (C and D) shows the sub-epithelial tissue comprising of haphazard arranged skeletal muscle fibers, nerve bundles, dilated and congested vessels of variable thickness and salivary ducts, a few mucinous glands; E) Photomicrograph E shows the sub-epithelial tissue comprising of haphazard arranged skeletal muscle fibers, nerve bundles, dilated and congested vessels of variable thickness and salivary ducts, a few mucinous glands.
Final diagnosis: Hamartoma of tongue
Discussion
Hamartoma is a relatively uncommon lesion in head and neck lesions, especially in younger children. Although hamartoma is not a true neoplasm, it behaves in a tumor-like manner in many ways. The term hamartoma should be used only when there is definite evidence of a developmental anomaly. The patients with sublingual hamartomas are asymptomatic and the treatment of choice is complete surgical excision. After the tumor mass is completely removed, there is no possibility of recurrence. Sublingual hamartomas are difficult to diagnose, because various clinical presentations and biopsies from non-representative sites may lead to a false diagnosis or no conclusion. According to the various studies and the available literature, the histopathological examination, therefore, plays an important role in the final diagnosis. So was it in our case. However, the criteria for separating hamartoma from other similar disease conditions are unclear.4 The findings in this report and previous literature suggests that hamartoma of the oral cavity requires a careful and multistep approach to achieve a favorable outcome and easy recovery of the patients.6
Conclusion
Finally, hamartomas should always be included in the differential diagnosis of the tumors of the oral cavity, mainly in the pediatric tumors, to avoid aggressive treatment and morbidity.4 Therefore histopathological correlation becomes necessary for definitive diagnosis.6
