Introduction
Human papilloma virus infection (HPV) causes more than 90% of cases of cervical carcinoma.1, 2 Most people who have had HPV infections, however, do not develop cervical cancer.3, 4 Other risk factors include smoking, weak immune system, birth control pills, multiple sexual partner. Invasive cervical cancer typically develops from precancerous changes over 10 to 20 years.4 Diagnosis is typically done by cervical screening followed by a biopsy. Medical imaging is then performed to determine whether or not the cancer has spread.
The value of histological and immunocytochemical assessments for predicting the clinical course of cervical cancer remains controversial as some advocates the studies of cell size, tumour differentiation or presence of antigenic markers while some opposes them.5, 6, 7, 8 So, the increasing search for better biomarkers to screen for cervical neoplasia due to marked inter- and intra-observer variability in the interpretation of Pap smears and cervical biopsy specimens has led to the study of p16/INK4a and Ki-67 as valuable biomarkers to improve the sensitivity and specificity of these tests and aid in the diagnosis of equivocal cervical biopsies.
The biopsies of cervical cancer show a wide range (10-50%) of tumour cell nuclei which are labelled by Ki-67, which presumably reflects considerable variation in the growth fraction of these tumours. In addition the distribution of nuclear labelling and hence proliferative activity varied within individual cases with central areas showing cell maturation and keratinization displaying little or no staining compared with the more actively proliferating peripheral portions.6 P16 immunostaining combined with Ki-67 can increase the diagnostic accuracy of high grade CIN and that p16 and Ki-67 are complementary biomarkers. p16 over-expression is an early event and Ki-67 works during the progression of CIN.9 The present study was carried out to study the expression of Ki-67 and p16 in neoplastic lesions of uterine cervix and to evaluate the prognostic significance of tumour differentiation, histological type, stage and grade, depth of tumour invasion and lymphovascular invasion in women with neoplasia of uterine cervix.
Materials and Methods
This study was performed on 120 biopsies and surgically resected specimens of uterine cervix. For histopathological study, specimens were fixed in 10% formalin, grossed, processed and paraffin embedded. Sections of 3-5 microns thickness was cut, stained with hematoxylin and eosin stains and was studied under light microscopy. Additional sections of 3-4 microns thickness were cut, placed on glass slide coated with poly L-lysine and immunohistochemical staining by p16 and Ki-67 was performed.
Immuno-expression of IHC p16 was based on the percentage of positively stained tumour cells: Negative: < 5%, Weak positive: 1+ (5%-25%), Moderately positive: 2+ (26%-50%) and Intense positive: 3+ (> 50%). To determine the grade of Ki-67 expression, nuclei of 200 epithelial cells located across the whole epithelial layer was examined in a high-power field (*400). Ki-67 index, defined as the percentage of Ki-67 positive cells was evaluated as: Negative: < 5%, 1+: 5-25%, 2+: 26-50% and 3+: >50%. Positive control in our study was tonsils for Ki67 and squamous cell carcinoma for p16 and the negative control was tissue without the primary antibody.
The response to treatment was assessed on follow up of patients at 3 months, 6 months and 12 months by clinicoradiological examination like CT scan, ultrasonography, colposcopy and other relevant lab investigations. For statistical analysis, all data were tabulated and analysed and appropriate statistical tests (chi square test and unpaired t test) was applied wherever necessary. 'p' values <0.05 was considered as statistically significant.
Observations
Majority of cases of invasive carcinoma cervix were large cell non-keratinizing squamous cell carcinoma, 58 cases (48.2%) followed by large cell keratinizing squamous cell carcinoma, 29 cases (24.6%). Among premalignant lesions 16 (13.2%) cases were of low- grade intraepithelial lesion (LSIL) and 6 (5.0%) were of High- grade intraepithelial lesion (HSIL) (Table 1).
Majority of cases of invasive carcinoma cervix were seen in stage 2B, 40 (40.8%) cases followed by stage 3B, 24 (24.4%) cases. Majority of the cases of squamous cell carcinoma were moderately differentiated, 58 (62.3%) cases, followed by well differentiated, 29 (31.2%) cases.
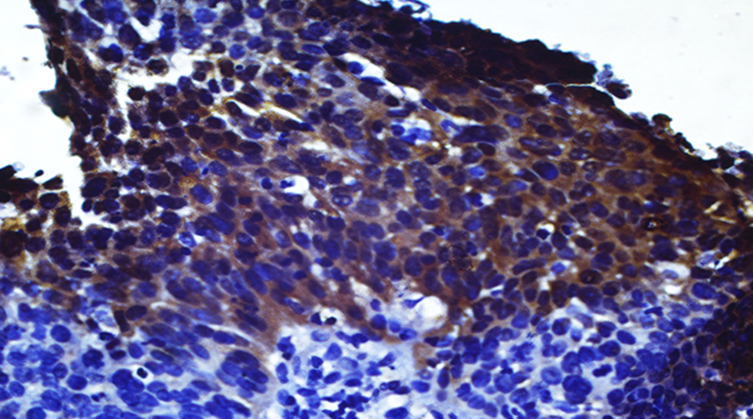
In 40 cases p16 immunomarker was applied. All the 6 (100%) cases of LSIL were negative. Out of 3 cases of HSIL, 2 (66.7%) showed 1+ positivity and 1 (33.3%) showed negativity. Out of 18 cases of large cell non-keratinizing squamous cell carcinoma, 12 (66.7%) showed 3+ positivity (Figure 1) and 6 (33.3%) showed 2+ positivity.
Figure 1
Large Cell Non-Keratinizing Squamous cell carcinoma (moderately differentiated squamous cell carcinoma): Photomicrograph shows intense cytoplasmic positivity with p16 antibody (score 3+). IHC p16x 40X.
Out of 9 cases of large cell keratinizing squamous cell carcinoma, 1 (11.1%) showed 3+ positivity, 2 (22.2%) showed 2+ positivity, 5 (55.6%) showed 1+ positivity and 1 (11.1%) showed negativity. The statistical correlation of IHC p16 immunoexpression and histological subtypes of cervical carcinoma was found to be significant (p <0.01) (Table 2).
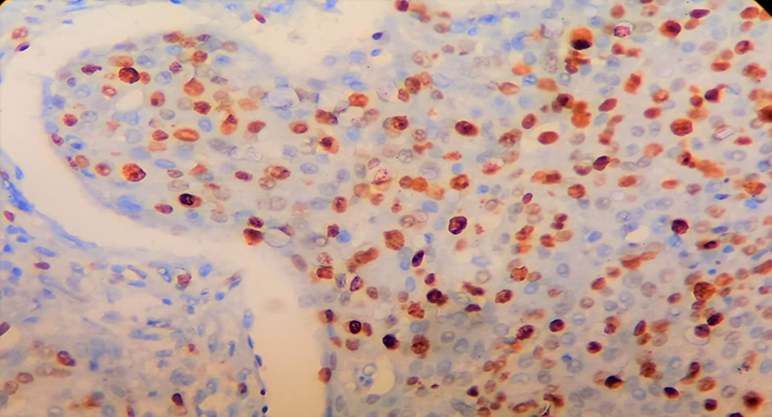
In 40 Cases, immunomarker Ki-67 was applied. All the 6 (100%) cases of LSIL were negative. Out of 3 cases of HSIL, 2 (66.7%) showed 1+ positivity and 1 (33.3%) showed 2+ positivity. Out of 18 cases of large cell non-keratinizing squamous cell carcinoma, 7 (38.9%) showed 3+ positivity (Figure 2), 4 (22.2%) each showed 2+ positivity and 1+ positivity and 3 (16.7%) were negative.
Figure 2
Large Cell Non-Keratinizing Squamous cell carcinoma (moderately differentiated squamous cell carcinoma): Photomicrograph shows tumour cells with Ki-67 antibodywith 3+ nuclear positivity. IHC Ki-67x 40X.
Out of 9 cases of large cell keratinizing squamous cell carcinoma, 3 (33.3%) showed 3+ positivity, 2 (22.2%) showed 2+ positivity, 1 (11.1%) showed 1+ positivity and 3 (33.3%) showed negativity. The statistical correlation of IHC Ki-67 immunoexpression and histological subtypes of cervical carcinoma was found to be insignificant (p >0.05) (Table 3).
Out of 13 cases of cervical carcinoma with stage 2A, 7 (53.8%) showed 3+ positivity, 3 (23.1%) cases each showed 2+ positivity and 1+ positivity for IHC p16. Out of 7 cases with stage 3A disease, 1 (14.2%) showed 3+ positivity, 3 (42.9%) cases each showed 2+ positivity and 1+ positivity. Both stage 1A and 4A showed 100% 3+ positivity for IHC p16. The statistical correlation of IHC p16 with stage of disease was found to be insignificant (p>0.05.
Out of 13 cases of cervical carcinoma with stage 2A, 5 (38.4%) showed 3+ positivity, 2 (15.4%) showed 2+ positivity, 3 (23.1%) cases each showed 1+ positivity and negativity for IHC Ki-67. Out of 8 cases with stage 3A disease, 3 (37.5%) showed 3+ positivity, 1 (12.5%) showed 2+ positivity and 4 (50.0%) showed negativity for IHC Ki-67. The statistical correlation of IHC Ki-67 with stage of disease was found to be insignificant (p>0.05).
Out of 19 cases of moderately differentiated squamous cell carcinoma, 12 (63.2%) showed 3+ positivity, 6 (31.6%) showed 2+ positivity and 1 (5.2%) showed 1+ positivity of p16. Out of 9 cases of well differentiated squamous cell carcinoma, 1 (11.1%) showed 3+ positivity, 2 (22.2%) showed 2+ positivity, 5 (55.6%) showed 1+ positivity and 1 (11.1%) showed negativity. A single case (100%) of poorly differentiated squamous cell carcinoma showed 3+ positivity. The statistical correlation between IHC p16 with histological grade of squamous cell carcinoma found to be significant (p<0.05) (Table 4).
Out of 19 cases of moderately differentiated squamous cell carcinoma, 7 (36.8%) showed 3+ positivity, 4 (21.1%) showed 2+ positivity and 5 (26.3%) showed 1+ positivity of Ki-67. Out of 9 cases of well differentiated squamous cell carcinoma, 3 (33.3%) showed 3+ positivity, 2 (22.2%) showed 2+ positivity, 1 (11.1%) showed 1+ positivity and 3 (33.3%) showed negativity. A single (100%) case of poorly differentiated squamous cell carcinoma showed 3+ positivity. The statistical correlation between IHC Ki-67 with histological grade of squamous cell carcinoma found to be insignificant (p>0.05) (Table 5).
Out of 30 patients on follow up, 19 (63.3%) patients were stable with no new complaint, normal blood and radiological investigations or were on ongoing treatment. 5 (16.7%) patients developed recurrence after having a disease free interval of 6-9 months. 6 (20.0%) patients developed metastasis in various organ after receiving cycles of chemotherapy and radiotherapy.
The correlation between IHC p16 and clinical follow up of patients were studied in 15 patients, in which 10 were stable, 3 showed recurrence and 2 had metastasis. Out of 10 stable patients, highest number of cases 4 (40.0%) showed negative p16 immunoexpression. All the 3 cases (100%) with recurrence showed 2+ positivity and 2 (100%) patients with metastasis showed 3+ positivity. The statistical correlation between IHC p16 and clinical follow up of patients was found to be significant (p<0.05).
The correlation between IHC Ki-67 and clinical follow up of patients were studied in 15 patients.10 were stable, 3 showed recurrence and 2 had metastasis. Out of 10 stable patients, highest number of cases 6 (60%) showed negative Ki-67 immunoexpression. All the 3 (100%) cases with recurrence showed 3+ positivity and one each (50.0%) patient with metastasis showed 2+ positivity and 3+ positivity (Figure 3).
Figure 3
Recurrence of squamous cell carcinoma: Photomicrograph shows tumour cells with Ki-67 antibody with 3+ nuclear positivity. IHC Ki-67x 40X.
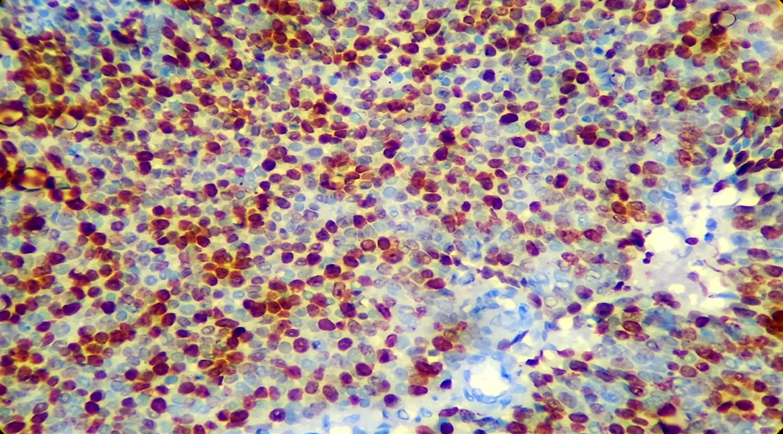
The statistical correlation between IHC Ki-67 and clinical follow up of patients was found to be significant (p<0.05).
Table 1
Distribution of cases according to histologic subtypes of cervical neoplasm.
Table 2
p16 immunoexpression in different cases of cervical neoplasms.
Table 3
Ki-67 immunoexpression in different cases of cervival neoplasms.
Table 4
Correlationof IHC p16 with histological grade of squamous cell carcinoma.
Table 5
Correlation of IHC Ki-67 with histological grade of squamous cell carcinoma.
Discussion
Majority of cases were found to be malignant in our study as compared to premalignant cases. Elsokary et al (2018) reported 27.3% precancerous lesions and 72.7% carcinoma cases [SCC 30 (75.0%), adenocarcinoma 10 (25.0%)] which are in accordance with our study.
In our study, majority of the cases of invasive carcinoma cervix were seen in stage 2B, followed by stage 3B. Kumar et al (2016) observed 55.33% of patients belonged to FIGO stage II disease which is in concordance with our study.10 But Eze et al (2013) found that the majority, 23 cases (56.1%), had advanced stage disease. (39.0% stage III and 17.1% stage IV), while stage I comprised only 9.8%.11
In our study, majority of cases of invasive carcinoma cervix were large cell non-keratinizing squamous cell carcinoma, followed by large cell keratinizing squamous cell carcinoma. Few cases of adenocarcinoma and adenosquamous carcinoma were also present. Among pre-invasive lesions, LSIL were higher in number than HSIL. In the study conducted by Kumar et al (2016), histology of the cervical cancer patients showed 91.8% squamous cell carcinoma, 3.5% adenocarcinoma and 1.67% adenosquamous cell carcinoma, which is in concordance with our study.10 Our findings are also in concordance with the study conducted by Chopra et al (2018) who concluded that carcinoma cervix have squamous carcinoma was the most common histology (91.4%) followed by adenocarcinoma or adenosquamous carcinoma or undifferentiated histology in 6.4% and 2.0% cases.12
Majority of the cases of squamous cell carcinoma were of moderately differentiated, followed by well differentiated, in our study. The study conducted by Shruti et al (2014) concluded that out of 199 patients, 109 (54.8%) had moderately differentiated, 51 (25.6%) poorly differentiated, 35 (17.6%) well differentiated squamous cell carcinoma and adenocarcinomas numbered only 4 (2.0%), findings in concordance with our study.13 Kalyani et al (2020) found that majority of cases had well differentiated squamous cell carcinoma followed by moderately differentiated squamous cell carcinoma which is discordant with our study.14
In our study, 100% cases of LSIL were negative for IHC p16 while 66.7% cases of HSIL showed 1+ positivity and 33.3% were negative. In invasive cases, out of 18 cases of large cell non-keratinizing squamous cell carcinoma, 66.7% cases showed 3+ positivity and 33.3% showed 2+ positivity. The study conducted by Kalyani et al (2020) found that out of 75 cases of squamous cell carcinoma of cervix, p16 biomarker expression was block positive, ambiguous and negative in 67 (89.3%), 5 (6.6%), and 3 (4.0%) cases, respectively.14 Mary (2017) concluded that p16 showed only 21.0% positivity in CIN-I lesions whereas in high grade dysplasia the positivity was above 60.0%.15 Sangwaiya et al (2018) concluded that p16 showed positive correlation with higher grade lesions.16 All studies are in concordance with our study.
Our study showed 100.0% cases of LSIL to be negative for IHC Ki-67 while 66.7% cases of HSIL showed 1+ positivity and 33.3% showed 2+ positivity. In invasive cases, among large cell non-keratinizing squamous cell carcinoma, 38.9% were showing 3+ positivity, 22.2% cases each showed 2+ positivity and 1+ positivity and 16.7% were negative. Sarwath et al (2017) found that 61.0% of squamous cell carcinoma and adenocarcinoma cases were positive for Ki-67.17 The degree of differentiation in their study, an important classification in squamous cell carcinoma cases revealed that the majority of samples were of non-keratinizing 68.8% (n = 53) subtypes, 26.0% (n = 20) were keratinizing carcinomas which are in concordance with our study. Hebbar et al (2017) concluded that invasive carcinomas showed diffuse and strong expression of Ki-67 in all cases.18 The overall agreement of Ki-67 staining with H and E diagnosis was 88.0% (κ = 0.595, P = 0.000022) which is in discordance with our study.
In our study, both stage 1A and 4A showed 100.0% 3+ positivity for p16. In cervical carcinoma with stage 2A disease, 53.8% showed 3+ positivity followed by equal number of cases (23.1% each) showed 2+ positivity and 1+ positivity for IHC p16. Kalyani et al (2020) concluded that there was no significant association between p16 expression and stage of the disease (p = 0.28).14 However, all stage I cases (100%) showed block positive p16 expression which are in concordance with our study.
In our study stage 1A showed equal number of cases with 3+ positivity and 1+ positivity for Ki-67 and stage 4A showed 100.0% 2+ positivity. In stage 2A disease, 38.4% showed 3+ positivity, 15.4% showed 2+ positivity followed by equal number of cases (23.1% each) showed 1+ positivity and negative for IHC Ki-67. The study conducted by Elsokary et al (2018) concluded that out of 13 cases with stage 1B, 2 (15.4%) showed 3+ positivity and 11 (84.6%) showed 2+ positivity.19 All 3 (100.0%) cases of stage 1A showed 2+ positivity and out of 5 cases of stage 2, 3 (60.0%) showed 3+ positivity and 2 (40.0%) showed 2+ positivity with p< 0.05 which is discordant with our study.
Out of 19 cases of moderately differentiated squamous cell carcinoma, 63.2% showed 3+ positivity for p 16, 31.6% showed 2+ positivity and 5.2% showed 1+ positivity. Out of 9 cases of well differentiated squamous cell carcinoma, 55.6% showed 1+ positivity followed by 2+ positivity (22.2%). 100% case of poorly differentiated squamous cell carcinoma showed 3+ positivity for p16. Kalyani et al (2020) concluded that majority of cases of well differentiated squamous cell carcinoma (88.0%) and moderately differentiated squamous cell carcinoma (93.7%) showed block positivity which is in accordance with our study.14
Out of 19 cases of moderately differentiated squamous cell carcinoma, 36.8% showed 3+ positivity for Ki-67, followed by 26.3% showed 1+ positivity and 21.1% showed 1+ positivity. Out of 9 cases of well differentiated squamous cell carcinoma, 33.3% showed 3+ positivity and 22.2% showed 2+ positivity. 100.0% case of poorly differentiated squamous cell carcinoma showed 3+ positivity. Elsokary et al (2018) reported that out of 9 cases of well differentiated squamous cell carcinoma, all 9 (100.0%) showed 2+ positivity.19 Out of 21 cases of moderately differentiated squamous cell carcinoma, 11 (52.4%) showed 3+ positivity and 10 (47.6%) showed 2+ positivity while all 10 (100.0%) cases of poorly differentiated squamous cell carcinoma showed 3+ positivity. Ki-67 expression showed statistically significant relation with high tumour grade (p-value = 0.017). This study is in discordance with our study.
In our study on follow up of 15 patients, 66.7% of cases were stable, 20.0% showed recurrence and 13.3% showed metastasis. Out of stable patients, highest number of cases (40.0%) showed negative p16 immunoexpression while 100.0% cases with recurrence showed 2+ positivity and 100.0% of cases with metastasis showed 3+ positivity. Schwarz et al (2012) concluded that the 5-year cause-specific survival was 33.0% for p16-negative cases (score = 0) compared with 63.0% for p16-positive cases (scores 1, 2, 3 or 4; p = 0.07).20 The 5-year recurrence-free survival was 34.0% for those who were p16-negative vs. 57.0% for those who were p16-positive (p = 0.09). This study is discordant with our study.
Out of stable patients, highest number of cases (60.0%) showed negative Ki-67 immunoexpression while 100.0% cases with recurrence showed 3+ positivity and 50.0% cases of metastasis showed 3+ positivity and 50.0% cases showed 2+ positivity. Kamer et al (2009) reported that during a median follow-up of 23 months, where radiotherapy was applied.21 Out of 17 patients 4 (23.5%) each developed local recurrence and distant metastasis. No significant correlation was detected among the local control and changes in Ki-67 index after receiving radiotherapy, whereas there was a moderate correlation between distant metastasis and changes in Ki-67 index after receiving radiotherapy (p = 0.01) in their study.
Conclusions
Scoring of p16 and Ki-67 increased with increase in grade of tumour. High scoring of p16 and Ki-67 is indicative of the high tumour proliferation and conversion into invasive tumour. Dual immunomarker positivity of p16 and Ki-67 tells us about disease progression, accordingly precise treatment to each patient can be planned.
