- Visibility 20 Views
- Downloads 3 Downloads
- DOI 10.18231/j.jdpo.2021.036
-
CrossMark
- Citation
A case of multiple spontaneous keloid scars: Letter to editor
- Author Details:
-
Lipika Behera
-
Shushruta Mohanty *
-
Swetambari Acharya
-
Chaitali Pattnaik
-
Deepika Mishra
Dear Sir,
A keloid scar is a benign hyperproliferative growth of dense fibrous tissue that extends beyond the borders of original wound. It results from abnormal healing response to cutaneous injury. For reaching at a diagnosis of keloid scar it is important to identify and elicit a history of injury prior to the occurrence of scar. Spontaneous keloid scar occuring in absence of any trauma or surgical procedure is rare. We therefore want to highlight about the fact that keloid can appear spontaneously and such cases are linked possibly to have a genetic etiology.
A 22-year short statured female presented to dermatology OPD with multiple cutaneous lesions present in the shoulder, upper arm and forearm since 10 years. The lesions were itchy, painful and gradually progressive over the years. On examination the lesions were firm, irregular shaped, hyperpigmented and erythematous with shiny surface. There was no history of any trauma prior to those lesions as informed by her mother. Her younger sibling who is 14 years old also complains of similar skin lesions in back and bilateral arms since 5 years. Thinking of a possibilty of any genetic etiology for such lesions in the family her mother was probed futher to give more detailed and relevant information about her. She was born at term by normal spontaneous vaginal delivery after an uncomplicated pregnancy. Her milestones were delayed, she left school at 5th grade due to learning diasbilities and as per her mother, who consulted a doctor at that point of time informed that her IQ was low. Other systems examined were unremarkable and her laboratory investigations were within normal limits. She was send to our cytology unit for FNAC. FNAC done showed bland looking spindle cells admixed with collagen bundles and sparse inflammatory cell infiltrate, no malignant cells seen. A biopsy taken from two different lesions showed features of typical keloid with nodular thick hyalinised collagen fibres in dermis sparing the papillary dermis. With features of short stature, delayed mile stones, low IQ with multiple keloidal lesions in absence of any trauma, and her younger sibling having similar skin lesions a possibility of some genetic etiology was thought over.


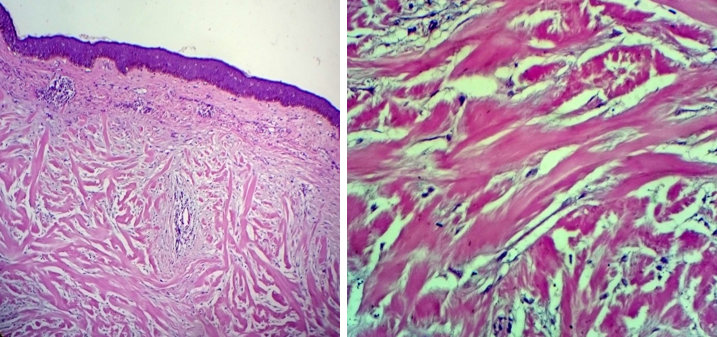
The term keloid dates from the 1800s and is derived from the Greek word ‘chele’, which means ‘crab claw’. This is because of the scar’s lateral extensions into normal tissue, which resemble the legs of a crab. Keloid scars are firm, broad erythematous nodules having shiny surface. They are frequently pruritic and painful and they do not regress naturally. Darker skin individuals are at greater risk of developing keloids in comparison with whites[1] and most common sites of predilection includes chest, shoulders, upper back extending to the neck and earlobes. keloids are generally reported frequently in lesions like acne, folliculitis, chicken pox and injectable vaccines and more obvious cause trauma due to ear piercing or post surgical intervention .Although pathogenesis is not clearly understood, keloids frequently occur following trauma or inflammation or after any surgical intervention. Etiology of keloid is possibly linked to genetic and environmental factors. Spontaneous keloid scar occuring in absence of any trauma is rare and has been reported in certain syndromes like Dubowitz syndrome, Rubenstein Taybi syndrome, Noonan syndrome, Geominne syndrome and conjunctivo-corneal dystrophy. [2], [3], [4], [5], [6] Histologically keloids are characterised by thickened hyalinised collagen bundles that are brightly eosinophilic with glassy fibres referred to as keloidal collagen.[7] Review of litertures have shown apart from these occurrences, single spontaneous keloid scar on the face has also been reported in two otherwise healthy men, in a 13-year-old on the preauricular region of the face and in an 81-year-old over the postauricular region.[8], [9]
Due to rarity of conditions resulting in spontaneous keloidal scar one needs to differentiate this entity from its closer mimics such as sarcoidosis and other benign and malignant tumours.[10] The findings of our patient, did not fit with any of the syndromes metioned above nor did it represent any syndrome in particular. There are various treatment modalities for keloid but those that are accepted widely includes intralesional steroid injections, cryotherapy, laser removal and radiotherapy.[11] Our patient had multiple such lesions on her body that resulted in cosmetic disfigurement that compelled her to seek medical attention. She was referred finally to a plastic surgeon for surgical excision and intralesional steroid treatment.
Conflict of Interest
There is no potential conflict of interests related to the exclusive nature of this paper.
Source of Funding
No financial support was received for the work on this manuscript.
References
- A E Brissett, D A Sherris. Scar contractures, hypertrophic scars, and keloids. Facial Plast Surg 2001. [Google Scholar] [Crossref]
- P Shilpashree, A K Jaiswal, PM Kharge. Keloids: an unwanted spontaneity in Rubinstein-Taybi syndrome. Indian J Dermatol 2015. [Google Scholar]
- M Paradisi, C Angelo, G Conti, S Mostaccioli, G Cianchini, F Atzori. Dubowitz syndrome with keloidal lesions. Clin Exp Dermatol 1994. [Google Scholar] [Crossref]
- AT Gulec, A Karaduman, D Seckin. Noonan syndrome: a case with recurrent keloid formation. Cutis 2001. [Google Scholar]
- L Goeminne. A new probably X-linked inherited syndrome: congenital muscular torticollis, multiple keloids, cryptorchidism and renal dysplasia. Acta Genet Med Gemellol (Roma) 1968. [Google Scholar] [Crossref]
- OH Haugen, T Bertelsen. A new hereditary conjunctivo-corneal dystrophy associated with dermal keloid formation. Acta Ophthalmol Scand 1998. [Google Scholar] [Crossref]
- J Y Lee, C C Yang, S C Chao, T W Wong. Histopathological differential diagnosis of keloid and hypertrophic scar. Am J Dermatopathol 2004. [Google Scholar] [Crossref]
- WHC Tiong, NH Basiron. Challenging diagnosis of a rare case of spontaneous keloid scar. J Med Cases 2014. [Google Scholar]
- C Monarca, M Maruccia, F Palumbo, P Parisi, N Scuderi. A rare case of postauricular spontaneous keloid in an elderly patient. In Vivo 2012. [Google Scholar]
- R Ogawa, S Akaishi, H Hyakusoku. Differential and exclusive diagnosis of diseases that resemble keloids and hypertrophic scars. Ann Plast Surg 2009. [Google Scholar] [Crossref]
- TA Mustoe, RD Cooter, MH Gold, FD Hobbs, AA Ramelet, PG Shakespeare. International Advisory Panel on Scar Management: International clinical recommendations on scar management. Plast Reconstr Surg 2002. [Google Scholar] [Crossref]
