Introduction
Central giant cell granuloma (CGCG) is a benign intraosseous proliferation which was first described in 1953 by Jaffe.1 It is most commonly seen in mandible or maxilla.2 WHO defines it as an intraosseus lesion consisting of cellular fibrous tissue that contains multiple foci of hemorrhage, aggregate of multinucleated giant cells and occasional trabeculae of woven bone.3 The presence of a co existent parathyroid adenoma and primary hyperparathyroidism is very rare.4 Here we report the unusual coexistence of both these entities in a 58years old man.
Case History
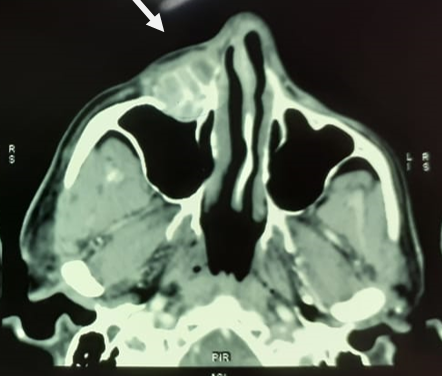
A 58 years old male presented with right cheek swelling since 3 months. On examination there was a firm mass over right upper cheek. CECT showed heterogeneously enhancing lesion with multiple hyperdense septation in the anterior wall of right maxillary sinus (size 41*30*23mm) with destruction of anterior wall (Figure 1).
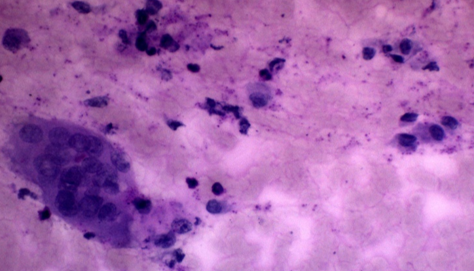
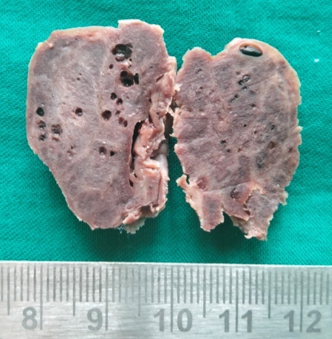
Following which FNAC from the swelling was done which showed scattered multinucleated giant cells with occasional mononuclear cells(Figure 2). Later the mass was excised via sublabial approach and we received a grey brown mass measuring 3.5*3*2.5cm, cut section of which was brownish with tiny cysts and thin bony septae in between (Figure 3).
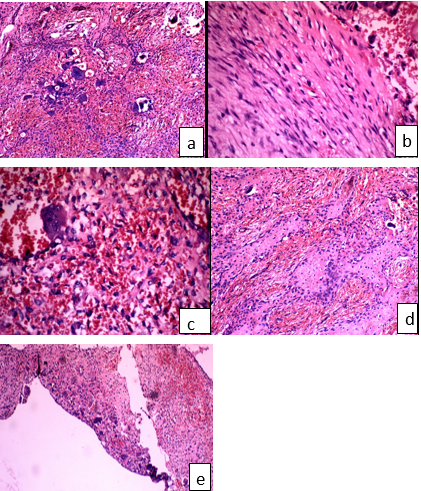
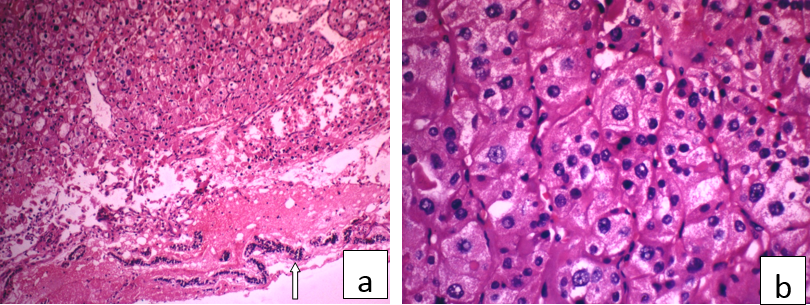
Microscopy showed diffusely arranged bland spindle cells and mononuclear stromal cells with extensive areas of hemorrhage. Multinucleated giant cells were seen mainly clustered around areas of hemorrhage and scattered singly. Frequent osteoid and new bone formation were also seen with focus of aneurysmal bone cyst like area (Figure 4a,b,c,d,e).
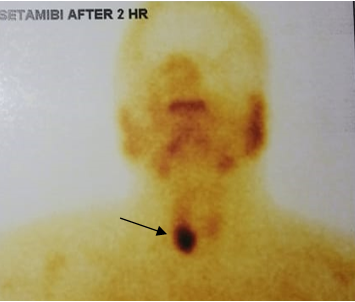
During the post operative period blood investigations showed a serum calcium of 13mg/dl(normal 8.8-10.6mg/dl), serum phosphorus of 3.80mg/dl(normal 2.5-4.5mg/dl), Alkaline phosphatase of 202U/L(normal 30-120U/L) and a Parathyroid hormone of 312pg/ml(normal 12-88pg/ml). Patient was further evaluated and a Technetium -99m MIBI parathyroid scan was done which showed MIBI avid lesion near lower pole of right lobe of thyroid suggestive of a parathyroid adenoma (Figure 5).
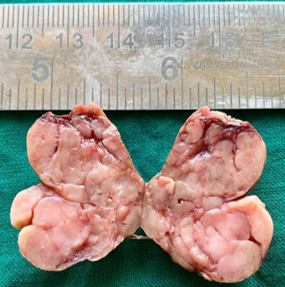
Few weeks later patient underwent parathyroid adenoma excision. The mass weighed 6.2grams and measured 2.8*2*1cm. Cut section was grey brown and lobulated (Figure 6).
Hematoxylin & eosin stained sections showed neoplasm composed of nests of chief cells and oncocytic cells surrounded by thin vessels. Occasional cells showed features of endocrine atypia. Periphery showed thin compressed parathyroid tissue (Figure 7a,b). Post operatively his serum calcium and parathyroid hormones became normal. On follow up patient is doing well.
Figure 1
CECT showing heterogeneously enhancing lesion with multiple hyperdense septation in the anterior wall of right maxillary sinus
Discussion
Coexistence of central giant cell granuloma of the maxilla and parathyroid adenoma resulting in primary hyperparathyroidism is rare. Gulati et al has reported a similar case where the giant cell lesion involved the posterior maxilla.4
In 1953, Jaffe described this entity as reparative granuloma of jaw bones.5 Clinical features include facial swelling, asymmetry and cortical plate expansion.6 Grossly the lesion is grey brown tan and often friable.2 Histology shows bland fibroblast like spindle cells in varying degrees of cellularity. Stromal cells may also be seen. Typically the giant cells are with lesser number of nuclei and are seen throughout the lesion but with clustering around areas of hemorrhage.2 Extensive hemorrhage, new bone formation, osteoid formation and secondary aneurysmal bone cyst like areas may be seen.2
Treatment usually consist of curettage or excision and recurrences are common in curetted lesions.4, 2
One of the close differential diagnosis would be a Brown tumour of hyperparathyroidism. Olvi et al decribes it as a lesion where the bone marrow will be replaced by richly vascularised connective tissue with giant cells and cancellous bone with surface osteoclastic activity in the periphery.7 In our case, clustering of giant cells around hemorrhage, reactive bone and osteoid formation and aneurysmal bone cyst like areas within the lesion favours central giant cell granuloma
Parathyroid adenomas are benign neoplasms composed of chief cells, oncocytes with frequent admixture of these cells. 8
Technetium 99m-Sestamibi is the commonly used radiotracer for imaging of parathyroid gland and is useful for preoperative localization of the lesion. Surgical excision of the adenoma is curative in majority of the cases.9
Conclusion
This case is being reported to highlight the fact that central giant cell granuloma (CGCG) can coexist with parathyroid adenoma. Endocrinology status of all patients diagnosed with CGCG should be assessed. Meticulous examination of the histological features may help to differentiate CGCG from its close mimickers