Introduction
Primary leiomyoma of ovary (PLO) are rare benign ovarian tumors which have an incidence of around 0.5-1%. They are mostly unilateral, small and asymptomatic tumors presenting between 20 to 65 years of age among which, around 85% are premenopausal.1, 2, 3 The possible origin of these tumors are from ovarian hilar blood vessels, ovarian ligament, metaplasia of cortical smooth muscles, undifferentiated germ cells or ovarian stromal smooth muscle cell.4
The tumor is most commonly diagnosed incidentally by histopathological examination and immunohistochemistry (IHC) of ovarian tissue after an ovariectomy for solid ovarian masses.
We present a rare case report of ovarian leiomyoma who was planned for laparotomy with a clinical diagnosis of subserosal uterine fibroid.
Case Report
Twenty three year oldunmarried girl presented in outpatient department with complaints of heaviness and mass in lower abdomen for 15 days. There was dull aching, non-radiating pain in lower abdomen with no associated bladder and bowel symptoms. She attained menarche at 15 years of age. Her menstrual cycles were regular with average flow along with mild dysmenorrhea. There was no significant past medical, surgical or family history.
She had average built with body mass index of 22.1 kg/m2. Nosignificant finding on general examination. On abdominal examination, a firm mass corresponding to gravid uterus size of 20 weeks was palpable which was non tender with smooth surface, regular margins and side to side mobile. The lower limit of mass was not reachable.
Abdominal Ultrasonography showed well defined hypo echoic mass measuring 11.5cm x 8.5 cm arising exophytically from the posterior wall of the uterus raising suspicion of subserous fibroid (Figure 1).
MRI pelvis was advised for further characterization of the mass lesion. It revealed large mass in the pelvis of size 18.2 cm x14.7 cm with left ovary not seen separately. The mass was hypo intense on T1 and T2 weighted images with small T2 hyperintense areas within it. Uterus was normal. These findings were radiologically suggestive of ovarian neoplasm (fibrothecoma) versus broad ligament fibroid (Figure 2 a,b,c).
In clinical board meeting, diagnosis of subserosal uterine fibroid was established. After routine preoperative investigations, she was planned for laparotomy. Per operatively a firm mass of 18 cm x 20 cm was seen with smooth surface and increased vascularity replacing the left ovary. Uterus, right ovary and both fallopian tubes appeared normal. There was no adhesions or any peritoneal fluid.
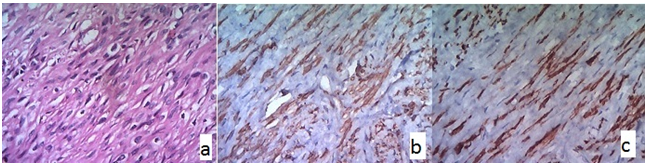
On gross examination, the tumor weighed 1.1 kg, was well encapsulated and cut surface was solid, firm, creamish white (with multiple tiny cystic areas, yellowish white nodules and foci of hemorrhage). The microscopic examination revealed intersecting fascicles of benign spindle cells with eosinophilic cytoplasm and bland elongated nuclei with blunt ends (Figure 3a). On IHC, neoplastic cells were diffusely positive for desmin and smooth muscle antigen (Figure 3b,c). The final diagnosis of leiomyoma of left ovary was made. No normal ovarian tissue could be identified.
The post-operative period was uneventful. Presently she has no complaints on a follow up period of one year.
Figure 1
Tranabdominal ultrasound revealing a large hateogenous, well define predominantly hypoechoic mass in left adnexal region.

Discussion
The first case of ovarian leiomyoma (OL) was described by Sangalli et al. in 1862. It appears to be most commonly reported from Eurasia.5 Most of these tumors do not cause any complaints and can be detected during a routine physical examination or incidentally during surgery or autopsy.6
OLs can be primary, secondary, or parasitic in origin. Primary Leiomyoma of ovary (PLO)are defined as lesions that originate from ovarian tissues (intraovarian blood vessels, smooth muscle fibers, or similar tissues within the ovarian stroma and tunica albuginea). 7 Secondary involvement of the ovaries can occur from intravenous leiomyomatosis or from leiomyomatosis peritonealis disseminata. 8 Parasitic OLs are extraovarian in origin, often originating from a pedunculated uterine leiomyoma that detaches and gets attached to the ovary.7, 9, 10 The incidence of primary ovarian leiomyomas is particularly low. 7
Usually, these are small measuring only few millimetres or centimetres in diameter, though few have reported large sized tumors too. Agarwal et al and Herbut et alreported large PLO of diameter around 20cm and 25 cm respectively. 11 In the present case, MRI findings revealed large mass of around 18 cm which is not a usual presentation for ovarian leiomyoma. The huge size could not clinch to the diagnosis of ovarian leiomyoma since these usually present as small sizes. Further, the clinical finding of side to side mobility favored subserosal uterine fibroid rather than broad ligament fibroid.
Majority of these tumors are asymptomatic due to small size. When symptomatic, they are related to the presence of the adnexal mass. Clinical presentations for symptomatic cases can be abdominal pain varying from mild to severe, palpable mass, acute symptoms due to torsion or necrosis or hydroureteronephrosis due to the great-size of the tumors. 12 In our case, patient presented clinically with abdominal heaviness and large abdominal mass, but it was not associated with any other symptom. In general, menstrual irregularities are rare in PLO and so was in our case.
Ovarian leiomyoma are often misdiagnosed preoperatively as pedunculated uterine myoma, ovarian fibroma or ovarian endometrioma. 7 In our case, USG revealed subserosal fibroid and MRI showed fibrothecoma or broad ligament fibroid. The final clinical diagnosis based on clinical examination and radiological reports, subserosal fibroid was established. On laparotomy, the present case had giant adnexal mass which was histopathologically confirmed to be PLO.
Differential diagnosis of leiomyomas and fibromatous tumors needs to be confirmed by immunohistochemistry. Desmin shows diffuse positivity in leiomyomas, whereas fibromatous tumors are typically negative or only focally positive.Smooth muscle antigen (SMA) is often positive in both leiomyomas and fibromatous tumors, but other stromal tumor such as cellular thecoma does not express SMA which express α-inhibin and calretinin. In the present case desmin and SMA were positive indicating the diagnosis of leiomyoma. 13, 14
Ovarian leiomyomas must be also differentiated from leiomyosarcoma. The microscopic features of the mitotic count, cytological atypia and tumor necrosis suggest the possibility of malignancy in a smooth muscle uterine tumor. 13 No signs of malignancy were evident on histopathological examination in the present case.
Ideally, a primary ovarian leiomyoma should be entirely within the ovary, with no similar lesions in the uterus or elsewhere. The co-existence of a ovarian leiomyoma with a uterine leiomyoma has been reported by several authors. 15, 16 There was no associated uterine leiomyomatosis in the present case. The ovary may become almost completely absorbed by the tumour, as in our case, or portions of it may pesist.17
Overall, these tumors have a benign course and surgical resection is the treatment.