Introduction
Osteomyelitis is an inflammatory process of bone and bone marrow caused by an infectious organism(s) which results in local bone destruction, necrosis and apposition of new bone.1 The etymology of the word osteomyelitis comprises the root word “osteon” meaning bone and “myelo” meaning marrow, combined with “itis” meaning inflammation.2 The aetiology of the disease is generally categorised into three main groups: hematogenous or blood borne spread, contiguous or direct contamination and vascular or neurologic insufficiency associated infection. 3 Hematogenous spread may be a result of a bacterial emboli migrating to the host bone from a distant source while blood acts as the carrier. It most commonly occurs in children and is usually caused by Staphylococcus aureus. Contiguous or direct spread is more commonly seen in adults and occurs by spreading to the bone from an adjacent soft-tissue infection. On the other hand, osteomyelitis due to vascular or neurologic insufficiency affects the older age groups more. 4 Osteomyelitis affects the elderly due to increased incidence of pre-existing high-risk conditions such as type 2 diabetes mellitus causing peripheral neuropathy and microangiopathy, peripheral vascular disease, and poor dentition. Surgical procedures like open-heart surgery, dental extractions, and prosthetic joint replacement, contribute to the causes as they are frequently performed in the elderly population. 5 Osteomyelitis could also be a result of bacterial infection post trauma. 4
Bone infections can be caused by any type of microorganisms, including bacteria, viruses, fungi and even parasites. But they are most commonly caused by certain pyogenic bacteria and mycobacteria.6, 7 Staphylococcus aureus (S. aureus) is the most common organism involved and is responsible for 80% to 90% of the cases of pyogenic osteomyelitis.5, 6, 7 Staphylococcus epidermidis (S. epidermidis) resides in abundancy in the skin and predominately infects medical equipment, including orthopaedic hardware implants and catheters.6, 7 Cause of contiguous spread of osteomyelitis is polymicrobial whereas chronic infections that are seen in cases of fractures and ischaemic ulcers are caused by S. aureus, Gram-negative bacilli, anaerobic bacteria.8
Characteristic pathological features of the diseases include progressive destruction of bone and the formation of sequestrum or dead bone.2
In acute cases such as those that spread haematogenously, patients usually present with signs of acute infection such as fever, chills, pain, and local signs of inflammation including pain, redness, tenderness, swelling, warmth.3 When osteomyelitis spreads directly from an adjacent focus of infection without vascular insufficiency, patients often present with pain, fever, and purulent drainage from a traumatic or surgical wound. In cases where prosthetic materials are involved, the disease may present late with milder signs and symptoms.9 When osteomyelitis occurs in the presence of vascular or neurologic insufficiency, pain is usually masked due to neuropathy. The most common source of infection is from a nearby neuropathic ulcer and the bones usually involved are the small bones of the feet.2
To successfully treat the infection, an early diagnosis is crucial.3 It depends on various factors that include patient’s history, eliciting the clinical signs, laboratory findings, imaging, histopathological analysis. 10 A multidisciplinary approach is used for the management of osteomyelitis requiring assistance from radiologists, orthopaedic surgeons, microbiologists, vascular surgeons and physiotherapists.2
The different types of osteomyelitis require different modes of treatment. Classifying the infection based on aetiology and chronicity would help to decide whether medical or surgical therapeutic strategies should be used.3 Microbiological identification of the causative organism(s) and surgical debridement if necessary or prompt initiation of antibiotic therapy are the cornerstones of the treatment.5 While acute osteomyelitis can be resolved with just antibiotics, chronic osteomyelitis more commonly requires surgical debridement to remove necrosed bone. 3 The latest treatment protocol dictates oral therapy following intravenous treatment for patients with osteomyelitis from contiguous spread of infection: Amoxicillin-clavulanate 875 mg/125 mg PO q12h or. Ciprofloxacin 750 mg PO q12h plus clindamycin 300-450 mg PO q6h or. Levofloxacin 750 mg PO daily plus clindamycin 300-450 mg PO q6h.11 Initial injectable antibiotic therapy followed by compliant oral antibiotic therapy has also been shown to be effective in children. 5 The choice between oral and parenteral antibiotics is also dependent on other factors like patient compliance and the causative agent’s sensitivity to the drug. 12 Surgical intervention is required when the infection progresses to a chronic stage and hence, the cornerstone of treatment of chronic osteomyelitis is surgery. 13 Surgical treatment would include debridement of dead bone, restoration of vascularity, adequate soft tissue coverage and reconstruction.12 Various techniques have been used in surgery such as muscle grafts, the Ilizarov technique, and antibiotic bone cements etc.8 The need for surgical intervention for treatment and the type of surgical procedure used for the removal of the infectious focus is determined by the histopathological processing of the samples obtained. 14
Materials and Methods
A retrospective study was done after obtaining informed consent from the institute’s Institutional Ethical Committee. The period of study was of three years, spanning from 2015 to 2017. 52 synovial biopsy specimens of patients suffering from osteomyelitis were collected from the pathology case files. The tissue specimens were fixed in 10% formalin and embedded in paraffin. Serial tissue sections of each specimen were prepared. Sections were stained with hematoxylin and eosin (HE). They were microscopically reviewed for analyzing histopathological features and were then classified into different grades using a grading system involving five characteristic histological features. Each feature was given a score of 0–3 points each, based on their histological abundance/severity. The total scores were then calculated and compared.
Histological parameters
There were five histopathological features chosen to compare. They included the following:
A1 Osseonecrosis
A2 Soft tissue necrosis
A3 Granulocyte infiltrate
C1 Bone neogenesis/fibrosis
C2 Lymphocyte/macrophage infiltrate
The above parameters were given the following scores based on abundance/severity: 0= <10% (non-existent)1= 10-30% (mild)2= 30-50% (moderate)3= >50% (severe)
If the sum of A1 to A3 was more than or equal to 4, then the specimen was graded as acute osteomyelitis. If the sum of A1 to A3 and C1 to C2 was more than or equal to 6, then the specimen was graded as chronically florid osteomyelitis. If the sum of C1 to C2 was more than or equal to 4, then the specimen was graded as chronic osteomyelitis. If the sum of C1 to C2 was less than or equal to 4, then the specimen was graded as subsided osteomyelitis. If the sum of C1 to C2 was less than or equal to 1, then the specimen was considered to have no indication of osteomyelitis. 14
Results
It was observed that out of the 52 synovial specimens, 9 specimens were graded as acute osteomyelitis, 11 as chronically florid osteomyelitis, 20 as chronic osteomyelitis, 45 as subsided osteomyelitis, and the rest had no histopathological features of osteomyelitis (Table 1). The radiology findings showed that 10 specimens showed osteosclerotic lesions, 4 had osteolytic lesions, 7 had osteopenic lesions and 2 of them had both osteosclerotic and osteolytic lesions (Table 2). The serology findings revealed increased ESR values (>100mm/hr) in 3 of the specimens, increased WBC counts (>11,000 cells/mm³) in 8 specimens, increased neutrophil counts (>80%) in 3 specimens and increased lymphocyte counts (>40%) in 6 specimens (Table 3).
Table 1
Results
Table 1 summarises the results of histopathological analysis of synovial specimens of the patients suffering from osteomyelitis and classifying them into five different grades using the scores obtained.
Table 2
Radiology findings
|
Type of lesion |
Number of specimens |
|
Osteosclerotic |
10 |
|
Osteolytic |
4 |
|
Oseopenic |
7 |
|
Osteosclerotic + Osteolytic |
2 |
Table 2 differentiates the radiology findings of affected bones/joints of the patients suffering from osteomyelitis based on the type of lesion.
Table 3
Serology findings
|
Laboratory values |
Number of specimens |
|
Increased ESR value (>100mm/hr) |
3 |
|
Increased WBC count (>11,000 cells/mm³) |
8 |
|
Increased neutrophil count (>80%) |
3 |
|
Increased lymphocyte count (>40%) |
6 |
Table 3 lists four different laboratory findings of the patients suffering from osteomyelitis that include increased values of ESR (erythrocyte sedimentation rate), WBC (white blood cell) count, neutrophil count, and lymphocyte count.
Discussion
Progression of untreated osteomyelitis leads to prolonged chronicity and complications and hence, surgical intervention might be imperative.3 The “Schmidt 100% rule” states that resolution of the infection and relief from the symptoms can only be achieved by complete surgical removal of the infection focus.15
Statistics point out that periprosthetic joint infection (25%) and mechanical loosening (19%) were the most common reasons for revision total knee arthoplasties. Along with periprosthetic fracture, periprosthetic joint infection was associated with the highest costs for revision total hip arthoplasties and total knee arthoplasties.16
The basic pathogenesis of osteomyelitis is dependent on the development of an acute inflammatory reaction that affects the periosteum and spreads within the bone causing bone necrosis known as a sequestrum. As the disease progresses to the chronic stage, inflammatory cells and cytokines stimulate osteoclastic bone resorption, fibrous tissue formation, and the deposition of new reactive bone. It is known as an involucrum when the newly formed bone forms a sleeve of living tissue around the segment of devitalized infected bone. 17
Histopathology of acute and chronic osteomyelitis varies in terms of osseous changes, soft tissue changes and the pattern of inflammatory infiltrates: 14, 18
Osseous changes
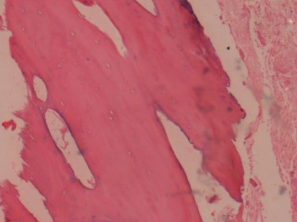
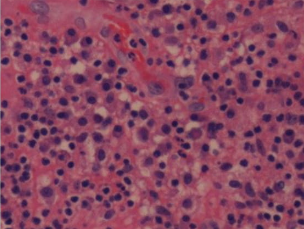
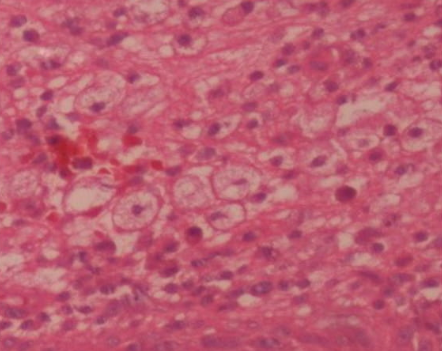
Osseonecrosis (Figure I) occurs in acute osteomyelitis where fragmented bone trabeculae with visually empty osteocyte cavities are detectable. Formation of new bone takes place in chronic osteomyelitis that comprises of spongy osseous tissue with reactive network bone neogenesis with osteoblasts bordering the bone surface. There is also fibroses with granulation tissue formation in the medullary space tissue.
Soft tissue changes
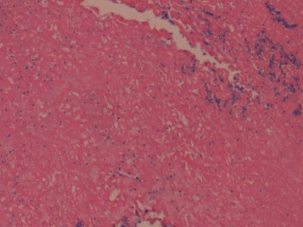
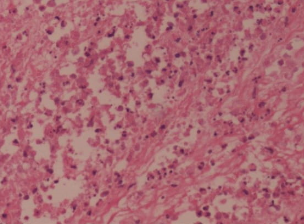
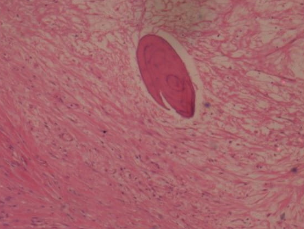
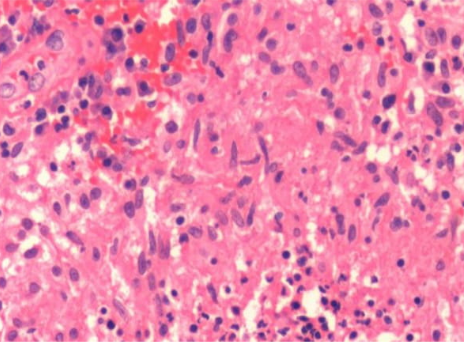
In the acute stages of infection, soft tissue necrosis (Figure II) is characterised by apoptoses, tissue eosinophilia, fibrin exudates and a confining texture of the tissue. As the disease progresses to the chronic stages, there is fibroses (Figure IV) with granulation tissue formation, the infiltrate consists of macrophages (Figure VI), lymphocytes (Figure V), plasma cells and a few neutrophilic granulocytes (Figure III).
Inflammatory infiltrate pattern
In acute osteomyelitis, diffuse and grouped deposits of segmented neutrophilic granulocytes (Figure III) in the usually highly oedematous medullary spaces are seen. Osteoclasts are also detectable alongside neutrophilic granulocytes on the irregular trabecular surface. On the other hand, lymphocyte/macrophage/plasma cell infiltrate is detected in the highly fibrosed medullary spaces of chronic osteomyelitis. 14 “Specific” osteomyelitis is defined by a histolopathological granulomatous inflammatory response (Figure VII) to specific pathogens, such as Mycobacteria, and hence, requires appropriate treatment. 18
Imaging plays a crucial role in diagnosis and follow-up of osteomyelitis. 2 The first imaging modality should always be conventional radiography to get an overview of the anatomy and the pathology underlying the involved bone and soft tissues. Sonography is useful in the diagnosis of fluid collections, periosteal and surrounding soft tissue involvement, and also provides guidance for diagnostic or therapeutic aspiration, drainage, or tissue biopsy. Computed tomography scan is less sensitive than other modalities for the detection of bone infection. The most sensitive and most specific imaging technique would be magnetic resonance imaging. It not only displays accurate anatomical spread of infection but also provides detailed information about the soft tissue involvement. 19 In adults, MRI has high diagnostic accuracy [95.6% sensitivity, 95% confidence interval (CI) 92.4% to 97.5%; 80.7% specificity, 95% CI 70.8% to 87.8%]. Due to its wider availability and zero exposure to ionising radiation, MRI is supposed to be the most preferred imaging modality. 20 Multifocal osseous involvement can specifically be detected with the help of nuclear medicine. 19
Laboratory tests can indicate infection but are usually nonspecific for osteomyelitis. 2 Laboratory findings in osteomyelitis include increased acute phase reactants levels like erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) and leucocytosis. 21 Although, the ESR and CRP are often elevated, they both lack specificity.2 CRP maybe more reliable than ESR for assessing response to treatment in children. 22
Prompt diagnosis can help in early resolution of the disease and hence, prevent the need for surgical intervention and lower the cost burden. An important step involved in the process of treating osteomyelitis is obtaining a sample from the diseased bone for microbiological and pathological examination to allow targeted antibiotic therapy. 3 A better understanding of pathophysiology underlying the disease is a key factor for development of better therapeutic strategies. 1
Conclusion
This analysis helped to confirm the diagnosis as well as classify osteomyelitis based on its histopathological features. The study also helped better the understanding of histopathology and compare the histologic variation present in synovial membrane tissue in patients suffering from different grades of osteomyelitis.