Introduction
Epithelial ovarian cancer generally presents with already advanced disease at the time of diagnosis and is accompanied by poor prognosis with increased mortality.1 Ovarian cancer is responsible for almost half of deaths from cancer of the female genital tract because malignant tumours often spread outside the ovary by the time a definite diagnosis is made.2
They spread predominantly directly within the pelvis and abdomen, but lymphatic and hematogenous spread may also occur.3 The most common sites of distant metastasis are the pleura, liver, lung and lymph nodes.2, 4 However bony metastases from ovarian cancer are rare. They tend to affect the axial skeleton and are associated with abdomino-pelvic disease.3 Median survival of patients with bony metastasis from ovarian malignancy ranges from 4 to 8 months.5, 6 Therefore early diagnosis and optimal management is crucial.
Case Report
A 49-year-old woman presented to the Orthopaedics Clinic with complaints of pain and swelling around the left knee joint since 2 months. Her appetite was decreased and she had mild abdominal pain for the same duration. There was no history of menstrual irregularities. On examination, there was absence of a left ankle jerk, with left sciatic-nerve irritation but no sensory or motor abnormalities. Her built was normal with no pallor or icterus. On abdominal examination, mild ascitis was noted with no appreciable organomegaly or lymphadenopathy.
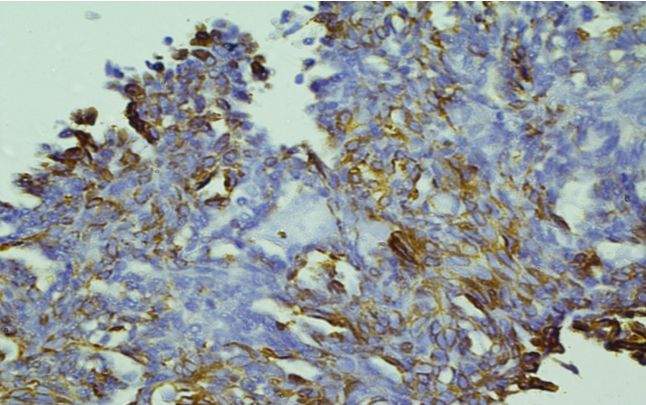
X ray of left leg showed a diffuse soft tissue swelling around the knee joint with focal cortical destruction. MRI examination showed foci of osteolytic lesions in the lower femur around the condyles. FNAC of the lesion revealed cohesive clusters of round to oval tumor cells with hyperchromatic nucleus and scant eosinophilic cytoplasm with nuclear moulding and crowding at places. At places acini formation was also appreciated (Figure 1). A cytologic impression suggestive of malignancy favouring metastatic adenocarcinoma was given. The patient was advised further investigations and a bone biopsy was performed. Subsequent ultrasonography of the lower abdomen showed a hypoechoic shadow in the left ovary. Left oopherectomy was performed under general anesthesia.
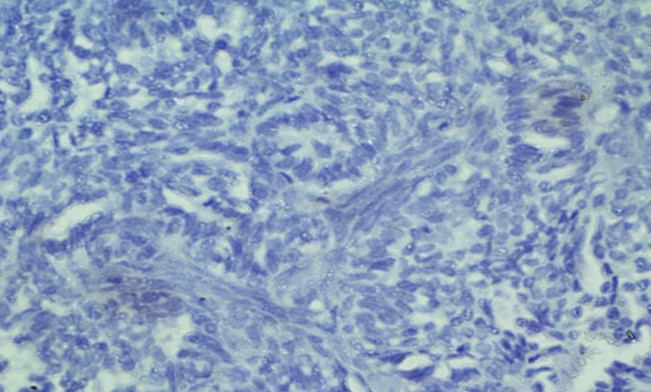
Grossly the ovarian mass was solid to cystic, 4.3x 3.5 cm in size and well encapsulated. Microscopically tissue sections showed papillary architecture of tumor, with minimal cytologic atypia lined by stratified round to oval tumor cells with hyperchromatic nucleus and mild eosinophilic cytoplasm (Figure 2). Immunohistochemical examination revealed strong nuclear positivity of tumors cells for estrogen receptor, diffuse membranous positivity for CK 7 (Figure 3) and PAX-8 (Figure 4) and negative immunoexpression for TTF-1 (Figure 5). The bone biopsy tissue examination revealed a similar morphological appearance and immunohistochemical phenotype to the left ovarian specimen. A final diagnosis of papillary adenocarcinoma of the ovary with femoral metastasis was made. She was treated with 6 cycles of combination chemotherapy of Paclitaxel 150 mg/m2 and Cisplatin 50 mg/m2 and a good response was seen. Our patient is doing well after 6 months of follow up period.
Figure 1
FNAC smears of the lesion revealed cohesive clusters of round to oval tumor cells withhyperchromatic nuceus and scant eosinophilic cytoplasm with nuclear moulding and crowding at places. At places acini formation was also appreciated. Hematoxylin and Eosin x 10X.
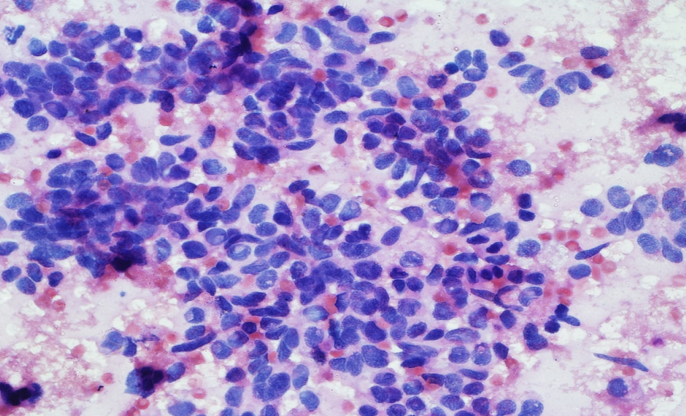
Figure 2
Microscopically tissue sections showed papillary architecture of tumor, with minimalcytologic atypia lined by stratified round to oval tumor cells with hyperchromatic nucleus and mild eosinophilic cytoplasm. Hematoxylin and Eosin x 10X.
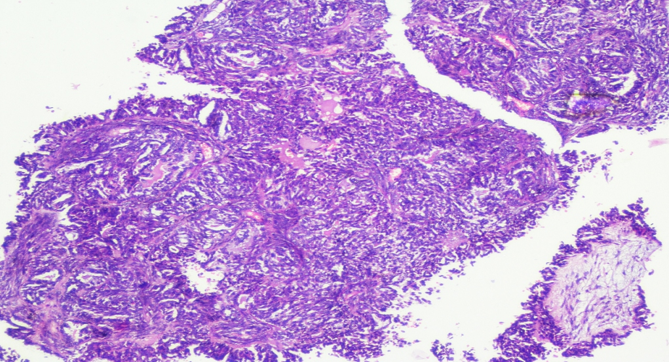
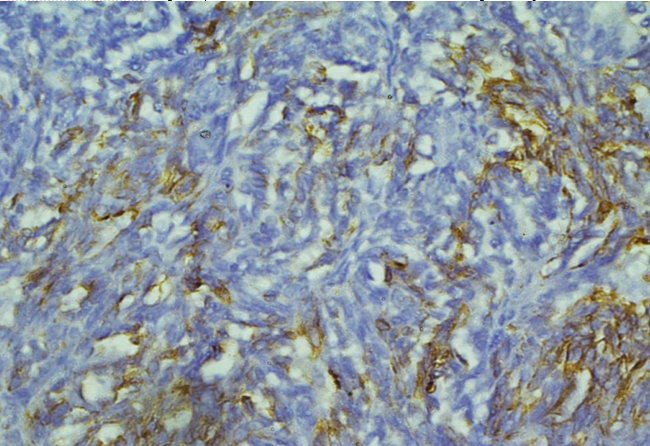
Figure 3
Immunohistochemical expression of CK 7 showed moderate membranous positivity of tumors cells. IHC CK7x10X.
Discussion
Ovarian cancer with bone metastasis is a rare condition with a poor prognosis. Pathological diagnosis of early bony lesions is essential in a case of ovarian cancer. Also systemic and local disease should be treated with early surgical intervention or palliative therapy for better survival of the patients.3
Ovarian cancer with extra-abdominal metastasis is rare and accounts about 3% of the cases.1 Several theories have been put forward to explain the occurrence of bony metastases in ovarian cancer. These include direct invasion from underlying growth, accidental implantation of tumor cells during surgery (iatrogenic), and through the lymphatics and hematogenous route.4, 5 Russel et al have reported four cases of bone metastasis in their study on 336 cases of epithelial ovarian cancer.3 The median time interval between diagnosis of epithelial ovarian carcinoma and presentation of bony metastases is 44 months.1 Seidman et al have reported 0.06-0.19% incidence of bony metastasis with epithelial ovarian cancer. 5 Barcena and Oliva have reported 7 cases of bony metastasis in 113 ovarian cancer patients.7 Bone metastasis was seen in high grades tumors only and the most common site observed was thoracic vertebra, followed by clavicle and axial skeleton.7 Cormio et al reported the incidence of distant bony metastases in stage IV ovarian cancer patients.8 Seidman et al had observed a greater incidence of bone metastasis in patients with positive pelvic and para aortic lymph nodes.5 The present case did not have any associated lymphadenopathy, but bony pain with secondaries was the first presentation.
Immunohistochemistry is essential for histologic diagnosis of suspected metastases, especially with an unknown primary.6, 7, 9 In women with a history of gynecologic tumor and papillary architecture of the metastatic foci, PAX8 is very helpful as it is specific marker for neoplasms of Müllerian duct origin.9 In our patient, possibility of primary thyroid cancer was excluded by negative immunoexpression of thyroglobulin, a marker highly specific of follicular thyroid neoplasms. Thus, we made a final diagnosis of metastatic papillary adenocarcinoma of the left ovary.
Effective chemotherapy for the treatment of ovarian carcinoma has prolonged patient survival.10 Besides chemotherapy, symptomatic management of extra-abdominal metastases should be considered. Surgical excision should be considered in selected patients after evaluating the patient's general condition. Bone lesions on the extremities may be safer to remove by surgery.11, 12
The bony metastases tend to appear late in the course of the disease with a poor prognosis and decreased survival.12, 13 Long-term surveillance should be continued in women with serous adenocarcinoma ovary as relapse after initial diagnosis has been reported to be as long as 28 years.14
Conclusions
This case highlights the importance of a thorough history, abdominal examination and investigations during orthopaedic admission so that such cases are not missed and patients mismanaged, especially as median survival is low with a rapid clinical deterioration. Pathologists and radiologists should not exclude primary ovarian carcinoma in a case of bony metastasis and long-term surveillance of women with epithelial ovarian cancer is recommended.