- Visibility 26 Views
- Downloads 8 Downloads
- DOI 10.18231/j.jdpo.2021.006
-
CrossMark
- Citation
Celiac disease in duodenal biopsies; 2 year experience at a tertiary care hospital
- Author Details:
-
Ritika Gupta
-
Sarojini Raman *
-
Bipad Bhanjan Mallik
-
Urmila Senapati
Introduction
CD (Celiac disease) is an autoimmune enteropathy, triggered by ingestion of proteins (gliaden, secalin) present in wheat, barley, rye and oats.[1], [2] The prevalence of celiac disease is 1.23% in northern, 0.10% in southern India and 0.87% in north eastern regions of India due to specific dietary habits in these regions.[3] Duodenal biopsies reveals mucosal damage classified according to Marsh-Oberhuber.[4] Serologic tests are essential for confirmation of such cases.[5] We have undertaken this study to analyse various histopathological features in suspected malabsorption cases in duodenal biopsies of CD cases in conjunction with clinical and laboratory parameters.
Materials and Methods
The present study was conducted in our institute from September 2018 to August 2020. During the two years study period, patients who presented to medical gastroenterology outpatient department with complaints of chronic diarrhea (diarrhoea lasting for more than four weeks), dyspepsia, fever, pain abdomen, vomiting, loss of appetite or weight loss, pallor due to anaemia, nutritional deficiencies (iron, folate, vitamin D), weakness underwent subsequent endoscopic biopsy of duodenum. So endoscopic duodenal biopsies of non neoplastic,suspected malabsorption cases with raised IELs were included in the study. Polyps and neoplastic conditions were excluded. Even inadequate biopsies those which were not properly oriented and tissue sections lost during processing were not taken. Multiple filter paper mounted duodenal specimen fixed in 10% buffered formalin were used. All tissues were embedded in paraffin blocks. 4-5µm thick sections taken and were stained with hematoxylin and eosin stain.
The different histopathological parameters studied were
Number of biopsy fragments received and site of biopsy.
Villous architecture- villous height (normal/broad or blunted)
Crypt architecture - crypt hyperplasia, crypt branching
Villous to crypt ratio-normal or less
Degree and composition of inflammatory cells in lamina propria. Degree of inflammation was graded as mild, moderate, marked.
Others- Surface ulceration, any exudate, reactive atypia, cryptitis, crypt abscess, fibrosis or any muscle disarray, lymphoid aggregate and granuloma.
Presence of any microorganisms like parasites (strongyloides, giardia) and tuberculosis etc were noted and confirmed by special stains like ZN stain for AFB
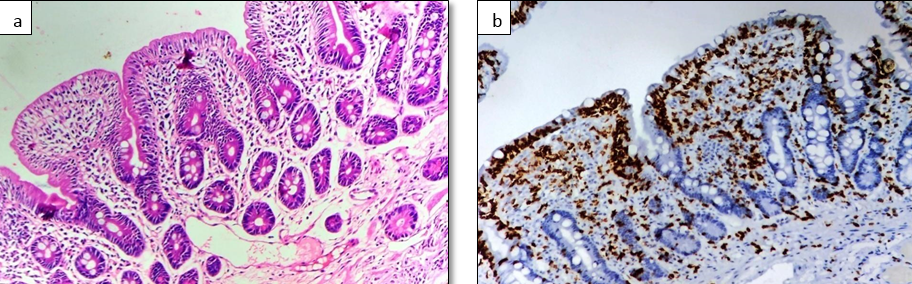
IEL: IELs were counted at villous tip and base of villi of properly oriented duodenal biopsies of the total 164 patients. Number of IELs per hundred enterocytes in five consequetive villi tip (twenty enterocytes in each villi) were counted. The upper limit of normal range for IEL: in villous tip = 20 IEL/100 enterocytes and at the base of villi = 18 IEL/100 enterocytes.[6] Immunohistochemistry (IHC) CD3 was done for all cases. The antibodies and chemicals were procured from Dako, Denmark (Rabbit Anti-CD3 Monoclonal Antibody (Clone EP41). The T lymphocytes take membranous positivity for CD3. Small intestinal tissue from resected specimens were taken as positive internal control.[6] Count was done similarly as in H and E stain. Other anciliary tests were correlated whenever possible. e.g.
Hematological- Complete blood count.
Serological- antitissue transglutaminase (tTG) IgA, tTG IgG tests.
Biochemical-Liver Function Test, Iron profile, Vitamin B12, folate assay
Stool test
Statistical analysis
The categorical variables were expressed as frequency and percentage.Quantitative variables with symmetrical distribution were expressed as mean ± SD and with asymmetrical distribution presented as median and range. To compare between categorical variables, either Chi - square test or Fisher‘s exact test was used and to compare between the quantitative variables, either independent T test or Wilcoxon Ranksum test was used based on the distribution of data. Statistical significance was defined as p < 0.05. All the analyses were carried out using a standard statistical software Stata 18.0.
Results
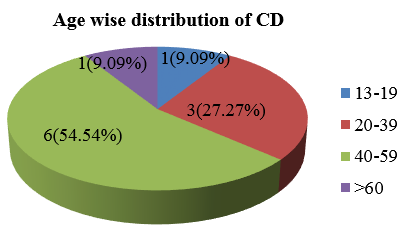
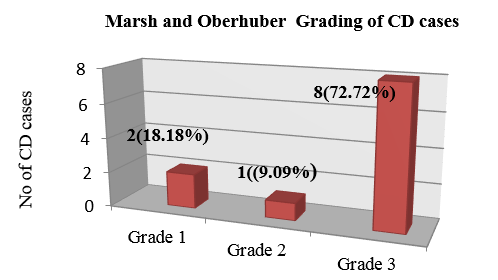
Total 164 cases of duodenal biopsies were studied. Out of which 105 cases had increased IEL histologically. Out of 105 cases, 11 cases were diagnosed as Celiac disease (CD). Rest were non celiac disease (NCD) of different aetiologies. Males (8,14.29%) are affected more than females (3,6.12%) by CD with a ratio of 2.6:1([Table 1]). The maximum cases of CD in our study group was in the age range of 40-59 years i.e 6(54.54%) cases. The mean age in CD cases in our study was 44.5 ± 14.49 years ([Figure 1]). There was no significant correlation between any of the symptoms in patients of celiac and non celiac disease. Pallor was present in only 5(20.83%) cases ([Table 2]). On comparison of laboratory parameters between CD & NCD cases Hb levels was found to be low in 5 (16.67%) cases of CD. LFT (liver function tests) were abnormal in 3 patients of CD. The laboratory parameters showing statistically significant correlation with CD were LFT(P~ 0.034). Serology (raised anti-Ttg,IgA,IgG) was raised in 11(100%) cases of CD ([Figure 3]). Majority of the CD cases 7(11.67%) had normal appearing mucosa in endoscopy. Scalloping was seen in 4(36.36%) of cases. None of CD cases had nodular and ulcerated mucosa. Our study had a significant statistical correlation between the endoscopy findings in CD (P~0.000) and NCD ([Table 4]). IEL at villous tip in H & E and CD3 was raised in all the CD cases. ([Figure 2] a,b). At base of villi in H & E it was raised in 5(4.76%) cases and in CD3 it was raised in 9(8.57%) cases thus increasing the diagnostic accuracy of CD ([Table 5]). In Celiac disease cases counting IEL at villous tip & base in H &E stain and IHC CD3, the mean IEL at tip of villi was higher than at base both in H& E (44.72 ± 26.9) and CD3 IHC stain (70±24.3) in CD cases. The sensitivity and specificity of detecting IEL by CD3 IHC is much more than H&E stain. The specificity of IEL at tip in CD is 100% in both H&E and CD3 IHC. It is 87.5% and 93.1% at base in H &E and CD3 respectively. Abnormal orientation was more in CD cases, ie. 5(10.64%) compared to NCD, 42(89.36%) cases. Architecture was normal in 5 (5.95%) cases of CD. Crypt architecture showed hyperplasia more in CD cases 8(61.54%). No cases of CD were having normal crypts. 2(4.08%) CD cases had crypt branching and 1 case showed distorted morphology. Blunting was seen in 8 (28.57%) cases of CD. Villous crypt ratio was normal (3:1) in 3 (3.90%) cases, 2:1 in 5(23.81%) cases and 1:1 in 3(42.86%) cases. Lamina propria inflammation was moderate in 11(100%) cases of CD. Architecture, crypt architecture, blunting, villous crypt ratio were showing statistically significant correlation with CD having (P~0.002), (P~0.000), (P~0,000) and (P~0.000) respectively ([Table 7]). Ulcer, exudates, parasite, crypt abscess, lymphangectasia, granuloma were almost absent in all the cases of CD. Reactive atypia, cryptitis and fibrosis were present in only 1(14.29%), 1(4.7%), 1(10%) cases of CD respectively. Edema was present in 6 (20.69%) cases. Lymphoid aggregate seen in 5(7.94%) cases of CD. Muscle disarray was present in 2 (16.67%) cases. None of these parameters had significant correlation with CD ([Table 8]). Among CD cases Only raised IEL was seen in 2 cases (Grade 1), Raised IEL with Crypt Hyperplasia in 1 case (Grade 2) and Raised IEL with Crypt Hyperplasia and Villous atrophy in 8 cases (Grade 3) according to Marsh oberhuber grading system ([Figure 3]).
|
Gender |
Celiac Disease(CD) |
Non Celiac Disease (NCD) |
P value |
Odds ratio |
|
Male |
8(14.29%) |
48(85.71%) |
0.173 |
0.391 |
|
Female |
3(6.12%) |
46(93.88%) |
|
Clinical parameters |
Celiac Disease (CD) |
Non celiac disease(NCD) |
P value |
Odds ratio |
||
|
1. |
Pallor |
Present |
5(20.83%) |
19(79.17%) |
0.059 |
3.28 |
|
Absent |
6(7.41%) |
75(92.59%) |
||||
|
2. |
Diarrhoea |
Present |
4(9.76%) |
37(90.24%) |
0.847 |
0.88 |
|
Absent |
7(10.94%) |
57(89.06%) |
||||
|
3 |
Abdominal Pain |
Present |
4(13.79%) |
25(86.21%) |
0.493 |
1.57 |
|
Absent |
7(9.21%) |
69(90.79%) |
||||
|
4 |
Loss of Weight |
Present |
2(10.53%) |
17(89.47%) |
0.994 |
1 |
|
Absent |
9(10.47%) |
77(89.53%) |
||||
|
5 |
Dyspepsia |
Present |
0 |
11(100%) |
0.225 |
1 |
|
Absent |
11 (11.96%) |
81(88.04%) |
||||
|
6 |
Loss of appetite |
Present |
0 |
2(100%) |
0.625 |
1 |
|
Absent |
11(10.68%) |
92(89.32%) |
||||
|
7 |
Fever |
Present |
1(33.33%) |
2(66.67%) |
0.190 |
4.6 |
|
Absent |
10(9.80%) |
92(90.20%) |
|
Laboratory Parameters |
Celiac Disease(CD) |
Non Celiac disease(NCD) |
P value |
Odds ratio |
||
|
1 |
Hb* |
Reduced |
5(16.67%) |
25(83.33%) |
0.190 |
2.3 |
|
Normal |
6(8.00%) |
69(92%) |
||||
|
2 |
ESR** |
Raised |
2(14.29%) |
12(85.71%) |
0.617 |
1.51 |
|
Normal |
9(9.89%) |
82(90.11%) |
||||
|
3 |
LFT† |
Raised |
3(30.00%) |
7(70.00%) |
0.034 |
4.66 |
|
Normal |
8(8.42%) |
87(91.58%) |
||||
|
4 |
Albumin |
Reduced |
2(22.22%) |
7(77.78%) |
0.229 |
2.76 |
|
Normal |
9(9.38%) |
87(90.63%) |
||||
|
5 |
Nutrition Deficiency |
Present |
3(27.27%) |
8(72.73%) |
0.055 |
4.03 |
|
Absent |
8(8.51%) |
86(91.49%) |
|
Endoscopy |
CD |
NCD |
P value |
Odds ratio |
|
Normal |
7(11.67%) |
53(88.33%) |
0.000 |
15.14 |
|
Scalloping |
4(66.67%) |
2(33.33%) |
||
|
Nodular |
0 |
15(100%) |
||
|
Ulcer |
0 |
24(100%) |
|
IEL count |
CD |
NCD |
|
|
Villous Tip (H&E) |
Raised |
11(10.4%) |
66(62.85%) |
|
Normal |
0 |
28(26.6%) |
|
|
Villous Tip (CD3, IHC) |
Raised |
11(10.4%) |
89(84.7%) |
|
Normal |
0 |
05(4.76%) |
|
|
Villous Base (H &E) |
Raised |
5(4.76%) |
52(49.52%) |
|
Normal |
6(5.71%) |
42(0.4%) |
|
|
Villous Base (CD3,IHC) |
Raised |
9(8.57%) |
67(63.80%) |
|
Normal |
2(1.90%) |
27(25.71%) |
|
IEL(CD) |
Villous Tip |
Villous Base |
||
|
|
H & E |
CD3 IHC |
H & E |
CD3 IHC |
|
Raised |
11(10.4%) |
11(10.4%) |
5(4.76%) |
9(8.57%) |
|
Normal |
0 |
0 |
6(5.71%) |
2(1.90%) |
|
Mean(±SD) |
44.72±26.9 |
70±24.3 |
41.1±45.1 |
36±30.05 |
|
Sensitivity |
14.3% |
11% |
8.77% |
11.8% |
|
Specificity |
100% |
100% |
87.5% |
93.1% |
|
PPV* |
100% |
100% |
45.5% |
81.8% |
|
NPV† |
29.8% |
5.32% |
44.7% |
28.7% |
|
|
Histological features |
CD |
NCD |
P value |
Odds ratio |
|
|
1 |
Architecture |
Normal |
5(5.95%) |
79(94.05%) |
0.002 |
0.158 |
|
Abnormal |
6(28.57%) |
15(71.43%) |
||||
|
2. |
Crypt architecture |
0.000 |
|
|||
|
a |
Normal |
0 |
36(100%) |
1 |
||
|
b |
Branching |
2(4.08%) |
47(95.92%) |
1 |
||
|
c |
Distortion |
1(14.29%) |
6(85.71%) |
3.91 |
||
|
d |
Hyperplasia |
8(61.54) |
5(38.46%) |
37.6 |
||
|
3 |
Blunting |
Present |
8(28.57%) |
20(71.43)% |
0.000 |
9.86 |
|
Absent |
3(3.90%) |
74(96.10%) |
||||
|
4 |
Ulcer |
Present |
0 |
4(100%) |
0.485 |
1.00 |
|
Absent |
11(10.89%) |
90(89.11%) |
||||
|
5 |
V/C Ratio |
0.000 |
|
|||
|
03:01 |
|
3(3.90%) |
74(96.10%) |
|
||
|
02:01 |
|
5(23.81%) |
16(76.19%) |
7.70 |
||
|
01:01 |
|
3(42.86) |
4(57.14%) |
18.5 |
||
|
6 |
Lamina propria inflammation |
0.076 |
|
|||
|
|
Mild |
|
0 |
15(100%) |
1 |
|
|
Moderate |
|
11(14.86%) |
63(85.14%) |
1 |
||
|
Severe |
|
0 |
16(100.00%) |
1 |
|
Other histological features |
|
CD |
NCD |
P value |
Odds Ratio |
|
|
7 |
Exudate |
Present |
0 |
2(100%) |
0.625 |
1.00 |
|
Absent |
11(10.68%) |
92(89.32%) |
||||
|
8 |
Parasite |
Present |
0 |
6(100%) |
0.388 |
1.00 |
|
Absent |
11(11.11%) |
88(88.89%) |
||||
|
9 |
Reactive atypia |
Present |
1(14.29%) |
6(85.71%) |
0.733 |
1.46 |
|
Absent |
10(10.20%) |
88(89.80%) |
||||
|
10 |
Cryptitis |
Present |
1(4.76%) |
20(95.24%) |
0.339 |
0.37 |
|
Absent |
10(11.90%) |
74(88.10%) |
||||
|
11 |
Crypt abscess |
Present |
0 |
5(100%) |
0.089 |
1 |
|
Absent |
11(11.00%) |
89(89.00%) |
||||
|
12 |
Edema |
Present |
6(20.69%) |
23(79.31%) |
0.100 |
3.54 |
|
Absent |
5(6.85%) |
68(93.15%) |
||||
|
13 |
Fibrosis |
Present |
1(10.00%) |
9(90.00%) |
0.965 |
1.04 |
|
Absent |
9(9.57%) |
85(90.43%) |
||||
|
14 |
Lymphoid Aggregate |
Present |
5(7.94%) |
58(92.06%) |
0.298 |
0.51 |
|
Absent |
6(14.29) |
36(85.71%) |
||||
|
15 |
Granuloma |
Present |
0 |
2(100%) |
0.625 |
1 |
|
Absent |
11(10.68%) |
92(89.32%) |
||||
|
16 |
Muscle disarray |
Present |
2(16.67%) |
10(83.33%) |
0.457 |
1.86 |
|
Absent |
9(9.68%) |
84(90.32%) |
Discussion
Increase in villous intraepithelial lymphocytes in duodenum when present whether carries significance or not is a matter of debate since last two decades. According to few authors it is nonspecific contradictory to few other studies. Though increased IEL with normal villous architecture is classified as grade 1 in CD, there are many other diseases with similar histologic findings. The specific diagnosis is difficult in many cases as in the preclinical stages of malabsorption minimal villous intraepithelial lymphocytes are seen.[5]
In a study done by Ian S. Brown et al in 150 serological positive for CD patients, age range at the time of diagnosis varied from 1 to 84 years, with 14.7% of patients aged 60 years or more. This reveals that CD can present can be in late age also. Similarly in our study 19 (18%) patient presented at later age i.e more than 60 years of age.[7]
Male: female ratio of CD in our study was 2.6:1. This is different from Priyavadhna et al and Ian S. Brown study. In both these studies ratio shows a female dominance though the reason for this is uncertain.[6], [7] Males and females were equal in number in a study of 60 CD cases by Mokhtar et al which also differs from our study. In our study there were only 11 cases of celiac disease. Number is too less to opine anything significant.[8]
11(6.6%) of CD cases were diagnosed in our study whereas in a South Indian study Priyavadhana et al (2017) founded 16 (15.8%) cases. Yadav P et al included 94 subjects in their study and reported CD in 61(64.9%).[4], [6] The high prevalence of CD may be primarily due to particular diet in Northern India in addition to increased awareness amongst people, better and sensitive screening techniques and recognizing the early changes in histopathology of biopsy specimen. In our study CD cases are less because of dietary habit and unawareness amongst the people.[4]
In CD cases of our study, anemia (pallor) was the most common presentation (5,20.83%), similar to Priyavadnam et al, Varma S et al, Mahadev et al.[6], [9], [10] In the present study mean Hb was 8.98±1.32 gm/dl, which was similar to Yadav P et al.(8.8 gm/dl) and Priyavadhna et al study (6.4 gm/dl).[4], [6] 3(2.85%) cases of CD presented with iron deficiency in current study. In contrast Priyavadhna et al (5,31.3%), and Yadav P et al(54, 88.5%) and Houria Chellat et al (29,6.63%) have reported IDA in more number of CD cases than ours.[4], [6], [11] Similar to present study Mahadev et al have observed no history of dietary sensitivities, allergies or history of intolerances to gluten or wheat containing products. None of their cases neither ours had a family history of gluten sensitive enteropathy.[10] LFT parameters was raised in 3(27.27%) patients of CD in our study. This correlates to observations by Rubio Tapia et al, Maggiore et al and Rostami-Nejad et al. They found raised transaminase level in celiac patients. This could be due to mild dyfunction of liver and a histological picture of nonspecific reactive hepatitis (known as celiac hepatitis) in CD cases.[12], [13], [14] Though LFT is deranged in some cases we have not studied the liver biopsy for correlation. In our study in 11(78.57%) out of 14 suspected CD patients, serology report was available. Out of these 11 cases a raised anti-Ttg was present in 7(0.50%) cases, raised IgA noted in one and IgG level was raised in 3 of the cases. Compared to this in Mahadev et al have reported only 3 of 11 patients had positive coeliac serology with positive anti-endomysial antibodies.[10]
In the present study in 11 cases of CD the mean of tip IEL in H & E was 44.72±26.9. It was much higher than mean of total raised IEL of total cases at 24±15.73. This is similar to S.Pellegegrino et al, Biagi F et al, Jarvinen TT et al, Mokhtar et al and Prasenjit Das et al.[8], [15], [16], [17], [18] Thus higher villous tip IEL points towards the suggestive diagnosis of CD. Contrary to this Shmidt et al have observed no correlation between CD and numbers of IELs. This variation in counts could be due to subjective differences in counting of IEL and use of IHC reduces this difference. The variation in counts can also be due to technical variations in thickness of histological sections.[19] In our study 89(94.6%) patients of non CD origin had raised IEL (villous tip) in CD3. Priyavadhana et al have demonstrated 37(36.6%) patients of non CD with increased IELs.[6] In cases of CD, in our series the sensitivity of IEL at tip in H &E was 14.3% and specificity was 100%. Goldstein and Underhill in their study found a high sensitivity (75%) but a low specificity (25%) contradictory to our study. [20]
In the present study villous blunting was present in 8(72.72%) out of 11 cases of celiac disease whereas blunting in Priyavadhana et al and Mokhtar et al was present in all cases of CD. In our study more number of cases of CD showed mild blunting (5,23.81%) whereas in their studies marked to complete villous atrophy were seen in more cases, 43.75% and >80% respectively.[6], [8] In present study villous flattening was not found in any of our CD cases similar to Goldstein and Underhill et al. 20 In our study crypt hyperplasia was present in both CD and NCD cases (in raised IEL cases ) whereas Priyavadhana et al observed crypt hyperplasia in patients of CD only and it was not a feature in NCD.[6]
Moderate degree of inflammation in CD was also observed in study of Malamut et al. But contrary to our study, Priyavadhana et al observed severe degree inflammation in CD.[6], [21]
In the present study of CD cases 8(72.7%) out of 11 were graded as Marsh 3.Similar findings in Mokhtar et al study where marsh 3 was the most reported grading for CD cases. This may be due to late presentation of cases, a result of unawareness of the disease among the general population.[8] In our study in cases of CD, no significant correlation was found between IEL and gender (p=0.391), clinical symptoms (p>0.05), and severity of inflammation in lamina propria (p=0.076) similar to a study by Mokhtar et al in CD cases.[8]
Advantage of our study
Our study emphasizes that the subtle histopathological changes in duodenal biopsies in correlation with robust clinical, biochemical, serological and endoscopic findings may be significantly useful in identifying many subclinical CD patients.
Limitation
Lack of serological testing for tTG (both IgA and IgG) as a screening tests in many cases due to unawareness and low incidence in the study group.
Conclusion
Celiac disease should be interpreted in association with complete clinical, histological and serologic work up. Endoscopic findings give significant initial clue for presence of CD and serological test are necessary for confirmation.
Source of Funding
No financial support was received for the work within this manuscript.
Conflict of Interest
The authors declare that they have no conflict of interest.
References
- D Schuppan. Current concepts of celiac disease pathogenesis. Gastroenterol 2000. [Google Scholar] [Crossref]
- A. Rubio-Tapia, J. A Murray. Classification and management of refractory coeliac disease. Gut 2010. [Google Scholar] [Crossref]
- B S Ramakrishna, G K Makharia, K Chetri, S Dutta, P Mathur, V Ahuja. Prevalence of Adult Celiac Disease in India: Regional Variations and Associations. Am J Gastroenterol 2016. [Google Scholar] [Crossref]
- P Yadav, P Das, B R Mirdha, S D Gupta, S Bhatnagar, R M Pandey. Current spectrum of malabsorption syndrome in adults in India. Indian J Gastroenterol 2011. [Google Scholar] [Crossref]
- E Ierardi, G Losurdo, A Iannone, D Piscitelli, A Amoruso, M Barone. Lymphocytic duodenitis or microscopic enteritis and gluten-related conditions: what needs to be explored?. Ann Gastroenterol 2017. [Google Scholar]
- P Balasubramanian, B A Badhe, R N Ganesh, L C Panicker, P Mohan. Morphologic Spectrum of Duodenal Biopsies in Malabsorption: A Study from Southern India. J Clin Diagn Res 2017. [Google Scholar]
- I S Brown, J Smith, C Rosty. Gastrointestinal Pathology in Celiac DiseaseA Case Series of 150 Consecutive Newly Diagnosed Patients. Am J Clin Pathol 2012. [Google Scholar]
- M Mokhtar, S O Mekki, H M Mudawi, S H Sulaiman, M A Tahir, M A Tigani. Histopathologic features of celiac disease in a sample of Sudanese patients. Malays J Pathol 2016. [Google Scholar]
- S Varma, P Malhotra, R Kochhar, N Varma, S Kumari, S Jain. Celiac disease presenting as iron-deficiency anaemia in northern India. Indian J Gastroenterol 2000. [Google Scholar]
- S Mahadeva, J I Wyatt, P D Howdle. Is a raised intraepithelial lymphocyte count with normal duodenal villous architecture clinically relevant?. J Clin Pathol 2002. [Google Scholar] [Crossref]
- H Chellat, M Salihoun, N Kabbaj, L Amrani, I Serraj, Z Chaoui. Diagnostic Yield of Routine Duodenal Biopsies in Iron Deficiency Anemia for Celiac Disease Diagnosis. ISRN Endoscopy 2013. [Google Scholar] [Crossref]
- A Rubio-Tapia, I D Hill, C P Kelly, A H Calderwood, J A Murray. American college of gastroenterology clinical guideline: diagnosis and management of celiac disease. Am J Gastroenterol 2013. [Google Scholar]
- G Maggiore, S Caprai. The Liver in Celiac Disease. J Pediatr Gastroenterol Nutr 2003. [Google Scholar] [Crossref]
- M Rostami-Nejad, T Haldane, D AlDulaimi, SM Alavian, MR Zali, K Rostami. The Role of Celiac Disease in Severity of Liver Disorders and Effect of a Gluten-Free Diet on Diseases Improvement. Hepat Mon 2013. [Google Scholar] [Crossref]
- S. Pellegrino, V. Villanacci, N. Sansotta, R. Scarfì, G. Bassotti, G. Vieni. Redefining the intraepithelial lymphocytes threshold to diagnose gluten sensitivity in patients with architecturally normal duodenal histology. Alimentary Pharmacol Ther 2011. [Google Scholar] [Crossref]
- P Das, G P Gahlot, A Singh, V Baloda, R Rawat, A K Verma. Quantitative histology-based classification system for assessment of the intestinal mucosal histological changes in patients with celiac disease. Intest Res 2019. [Google Scholar]
- T. T. Järvinen, P. Collin, M. Rasmussen, S. Kyrönpalo, M. Mäki, J. Partanen. Villous tip intraepithelial lymphocytes as markers of early‐stage coeliac disease. Scand J Gastroenterol 2004. [Google Scholar] [Crossref]
- F Biagi. Intraepithelial lymphocytes in the villous tip: do they indicate potential coeliac disease?. J Clin Pathol 2004. [Google Scholar] [Crossref]
- E Shmidt, T C Smyrk, C L Boswell, F T Enders, AS Oxentenko. Increasing duodenal intraepithelial lymphocytosis found at upper endoscopy: time trends and associations. Gastrointest Endosc 2014. [Google Scholar] [Crossref]
- NS Goldstein, J Underhill. Morphologic Features Suggestive of Gluten Sensitivity in Architecturally Normal Duodenal Biopsy Specimens. Am J Clin Pathol 2001. [Google Scholar] [Crossref]
- G Malamut, V Verkarre, F Suarez, J-F Viallard, A-S Lascaux, J Cosnes. The Enteropathy Associated With Common Variable Immunodeficiency: The Delineated Frontiers With Celiac Disease. Am J Gastroenterol 2010. [Google Scholar] [Crossref]
