- Visibility 156 Views
- Downloads 16 Downloads
- Permissions
- DOI 10.18231/j.jdpo.2021.005
-
CrossMark
- Citation
Expression of P16 and KI-67 in cervical intraepithelial neoplasia and carcinoma: An institute based study
- Author Details:
-
Nongmaithem Karuna Devi *
-
L. Sushila Devi
-
L. Ranjit Singh
Abstract
Background: Cervical cancer is one of the leading causes of cancer death in Indian women Cervical cancer screening programme worldwide are moving from primary cytology to human papilloma virus (HPV) DNA testing, which is the major risk factor for cervical carcinoma.
Objectives: To study the expression of P16 and KI-67 in cervical intraepithelial lesions and carcinomas and to calculate diagnostic accuracy of these biomarkers as compared to routine histopathology findings on equivocal cases
Material and Methods: Evaluation for p16 and ki-67 immunoexpression was done in 102 cervical tissue samples. Informed consent, details of the patient regarding age, occupation, religion, parity, symptoms, any prior abnormal pap test, HPV DNA test if any, etc. were taken before procuring the samples.
Results: The benign lesions were negative for both p16 and ki-67 immunoexpression whereas the premalignant lesions showed increasing positivity with the higher histological grade. All the malignant lesions were positive for ki 67 and p16 except for one case The specificity was highest when both the markers were used together.
Conclusion: Correlation of p16 and ki-67 biomarkers and histopathology findings increases the diagnostic accuracy of premalignant and malignant cervical lesions which may be useful in cases with equivocal histologic features
Introduction
Cervical cancer is one of the most common cancer in women though different parts of the world have varied incidence rate.[1] The incidence have now fallen in most of the developed countries. However, in most of the developing countries the incidence rate remain unchanged or have risen.[2] In 2018, India recorded 97,000 cases and 60,000 deaths which is the highest number of death due to cervical cancer.[3] With the recognition that virtually all cervical cancers are caused by infection with high risk(carcinogenic) HPV types, testing for HPV DNA are now developed to improve cervical screening strategies, which is widely accepted as a strategy to decrease the incidence of cervical cancer and mortality related to it.[4]
About 70% of cervical cancers are caused by HPV-16 and HPV-18 types and HPV-16 alone is responsible for 50% of all the cervical cancer worldwide. The expression of several host genes is affected by the oncogene products of HPV, including those involved in cellular proliferation, such as Ki-67 and cell cycle control, such as p16. Immunostaining for p16 is an effective biomarker of cervical disease.[5], [6] However, since some benign cervical epithelial cells can exhibit p16 expression, evaluation of p16 staining requires additional morphological evaluation.[7] Ki-67, a marker for cell proliferation, is particularly helpful in cases where p16 staining is inconclusive or technically inadequate.[8] Recently, a double- label immunostain for p16 and Ki-67 was developed that allows recognition of abnormal cells simply based on co-staining of the two markers in the same cell.
Aims and Objectives
To evaluate p16 & Ki-67 immunoexpression in cervical lesions and their utility in detection of CIN and cervical carcinoma
Materials and Methods
It is a Hospital based cross sectional study conducted from August 2018 to January 2020, consisting of 102 samples.
Inclusion criteria
All hysterectomy and the cervical biopsy cases irrespective of age during the study period
Exclusion criteria
Cervical biopsy and hysterectomy specimen with prior radiotherapy or chemotherapy, prior treatment for cervical diseases like cryotherapy, LASER therapy and loop electrosurgical excision process, pregnancy and patients who do not want to participate in the proposed study.
In addition, relevant clinical and personal history like age, marital status, symptoms, prior abnormal pap test, result of HPV genotyping, wherever available were recorded.
The cervical tissues were fixed in 10% buffer formalin, processed and sections of 3-5 micrometer thickness were prepared from the paraffin blocks, deparaffinised and stained with haematoxylin and eosin for light microscopy.
For immunohistochemical staining, sections of 3-5 micrometer thickness made in poly L Lysine coated glass slides were kept overnight at 30-35 degree Celsius, deparaffinised and rehydrated. Antigen retrieval was done by pressure cooker method after keeping the slides in TRIS buffer (pH 9) filled container for 3 minutes at approximately 120 degree Celsius. After antigen retrieval, the slides were washed with phosphate buffer solution (pH7.2-7.6), blocking reagents added, followed by addition of primary antibody, incubation at room temperature in humidity chamber for 30 minutes. After washing with PBS, secondary antibody was added, incubated again for 30 minutes and washed again with PBS. DAB chromogen are added to the slides and after 10 minutes, washed with distilled water which is followed by clearing and mounting.
Ki-67
Staining in the upper two third of the epithelium was scored as positive, using scores from 1 to 3.[9]
p16
Staining is nuclear as well as cytoplasmic and was scored as diffused if continuous staining is seen in the horizontal plane, either partial or full thickness. If staining is interrupted in this plane, it was scored as focal. Weakly diffuse staining, characterized by a “blush” was scored as negative.
Statistical analysis
The results obtained were entered in MS Excel and analysed using SPSS 22.version and the following statistical analysis were calculated:
Descriptive like mean, percentage and range.
Analytical statistics like Chi-square test etc.
The Sensitivity, Specificity, Positive Predictive value (PPV), Negative Predictive Value (NPV) and accuracy were calculated, where p <0.05 was considered as statistically significant.
Ethical Issue
Approval of the institutional ethics committee, was obtained, informed written consent was taken and confidentiality of the patient was strictly maintained.
Results and Observation
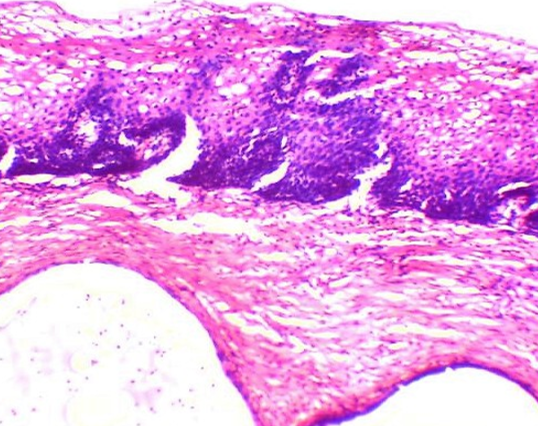
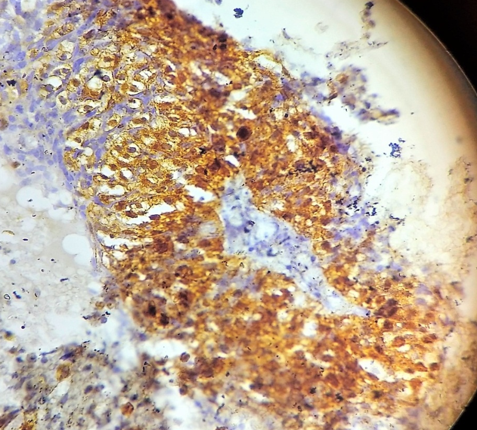
A total of 102 cases were studied with chronic cervicitis, CIN and malignancies accounting for 66 cases (64.7%), 31 cases (30.3%) and 5 cases (4.9%) respectively. Among the 31 cases of CIN, 19 were CIN I ([Figure 1]), 8 cases were CIN II and 4 cases were CIN III ([Table 1]).
|
S. No |
Diagnosis |
No. of cases |
Percentage |
|
1. |
Chronic cervicitis |
40 |
39.2% |
|
2 |
Chronic cervicitis with metaplasia |
26 |
25.5% |
|
3. |
CIN I |
19 |
18.6% |
|
4. |
CIN II |
8 |
7.8% |
|
5. |
CIN III |
4 |
3.9% |
|
6. |
Carcinoma |
5 |
4.9% |
|
|
Total cases |
102 |
|
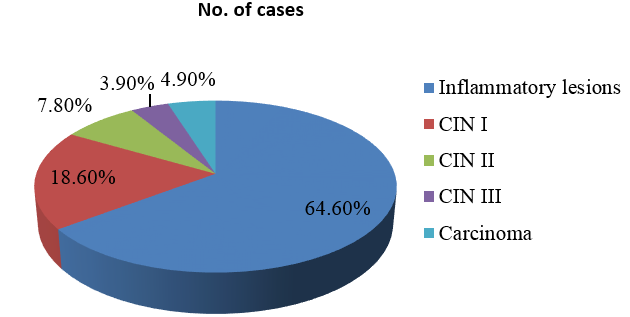
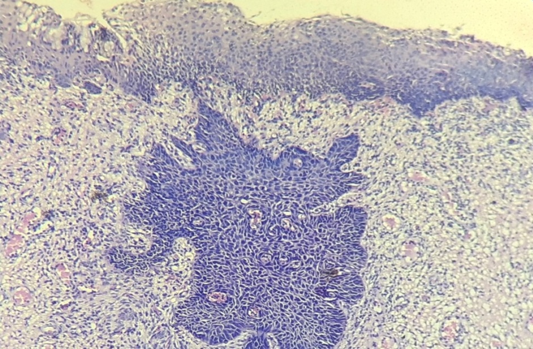
Amongst the 5 cases of carcinomas, 3 were moderately differentiated squamous cell carcinoma, ([Figure 2]), 1 case each of adenosquamous with neuroendocrine differentiation and basaloid variant of squamous cell carcinoma.
The age of the patients in the study as shown in table 3 ranged from 28 to 78 years with the mean age of 47.34 years. Majority of the cases were in age group of 40 to 49 years while most of the benign lesions were seen in the < 50 years age group and malignant cases were observed in the above 50 years age group. ([Table 2])
|
Age (years) |
chronic cervicitis |
Chronic cervicitis with squamous metaplasia |
CIN I/ II/ III |
Carcinoma |
|
20-29 |
1 |
0 |
0 |
0 |
|
30-39 |
9 |
4 |
4 |
0 |
|
40-49 |
23 |
10 |
17 |
1 |
|
50-59 |
5 |
7 |
6 |
4 |
|
60-69 |
2 |
5 |
3 |
0 |
|
70-79 |
0 |
0 |
1 |
0 |
Among the 31 cases of intraepithelial neoplasia 18(58%) cases and 5(100%) cases of carcinoma were multiparous (> 2 issues). Maximum clinical presentation was abnormal vaginal discharge as seen in 21(61.7%) cases of CIN and 3(60%) cases of carcinoma which was followed by abnormal vaginal bleeding. 13(42.9%) cases of CIN and 4(80%) cases of carcinoma had early age of marriage as shown in [Table 3].
|
I. Parity |
CIN I/ II/ III n (%) |
Carcinoma n (%) |
|
Multiparity (> 2 issues) |
18 (58%) |
5 (100%) |
|
1-2 issues |
13 (41.9%) |
0 |
|
Nulliparity |
0 |
0 |
|
II. Clinical symptoms |
|
|
|
Abnormal vaginal discharge |
21 (67.7%) |
3 (60%) |
|
Abnormal bleeding per vagina |
10 (32.3%) |
2 (40%) |
|
III. Age of marriage |
|
|
|
Early marriage(<20 years) |
13 (41.9%) |
4 (80%) |
|
Normal age (20-30 years) |
11 (35.4%) |
1 (20%) |
|
Late marriage(>30 years) |
6(19.4) |
0 |
Prior pap test were recorded in all cases of dysplasia and carcinomas. Out of 19 cases of CIN I, 5(26.3%) cases and 4(50%) cases out of 8 cases of CIN II were found to have abnormal pap test whereas all cases of CIN III and carcinomas had prior abnormal test.
Results of HPV test were available in 7 cases of CIN and 4 cases of carcinoma. HPV genotyping either 16 or 18 or both was detected in 2 (10.5%) cases of CIN I, 3(37.5%) cases of CIN II, 2(50%) cases of CIN III and 4(80%) cases of carcinoma
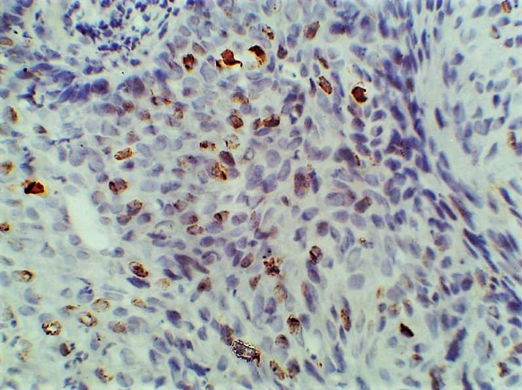
The p16 and ki-67 immunoexpression were evaluated in all the cases and correlated with the histopathological findings. ([Table 4]). In inflammatory lesions, no immunoexpression of p16was observed. Ki-67 expression in such lesions were also taken as negative as immunoexpression was not observed in the upper 2/3rd of the epithelium. Positive immunostain for p16 were observed in 26.3%, 50%, 75% and 80% of the cases of CIN I, CIN II, CIN III and carcinomas ([Table 4]) respectively. This may be due to association of HPV with high grade dysplastic lesions and malignancies of cervix. KI-67 immunostain was positive in all cases of carcinoma ([Table 4]) and in cases of CIN, the rate of Ki-67 positivity increases with increasing severity of dysplasia.. Both p16 and Ki-67 expression with various cervical lesions were highly significant as p < 0.05.([Table 4])
|
|
Positive p16 expression |
Positive ki-67 expression |
|
n (%) |
n (%) |
|
|
1.chronic cervicitis |
0 |
0 |
|
2.chronic cervicitis with metaplasia |
0 |
0 |
|
3.CIN I |
5 (26.3) |
6 (31.6) |
|
4.CIN II |
4 (50) |
5 (62.5) |
|
5.CIN III |
3 (75) |
4 (100) |
|
6.Carcinoma |
4 (80) |
5 (100) |
Majority of the cases (13 nos.) of CIN I lesions did not show ki-67 expression. Grade 1 ki- 67 positivity were seen in 4 cases of CIN I, 3 cases of CIN II and 2 cases of CIN III whereas 2 cases of CIN I, 1 case of CIN II, 2 cases each of CIN III and carcinoma showed grade 2 positivity. Grade 3 ki-67 immunostain were observed in 1 case of CIN II and 3 cases of carcinoma.
Grade 1 p16 immunostain were observed in 1 case of CIN I and 3 cases of CIN II whereas 4 cases of CIN I, 2 cases of CIN II and 2 cases of CIN III showed grade 2 positivity. Two cases each of carcinoma showed grade 2 and grade 3 p16 positivity which may point towards their aggressiveness. However, 1 case of carcinoma was negative for p16 immunostain.
The performance of p16 and ki-67 in determining the lesions ≥ CIN II were studied and the results are shown in [Table 5]. The specificity was highest when both the markers were positive i.e. 97.65%.
|
Immunostaining positive |
Sensitivity (%) (95% CI) |
Specificity (%) (95% CI) |
Accuracy (%) (95% CI) |
PPV (%) (95% CI) |
NPV (%) (95% CI) |
|
P16 |
76.47 (50.10-93.19) |
91.95 (84.12-96.70) |
80.77 (71.88-87.84) |
96.11 (92.04-98.14) |
60.08 (38.92-78.04) |
|
Ki-67 |
82.35 (56.57-96.20) |
92.94 (85.27-97.37) |
85.53 (77.18-91.71) |
96.46 (92.43-98.38) |
69.30 (44.66-86.33) |
|
Both p16 & ki-67 |
64.71 (38.33-85.79) |
97.65 (91.76-99.71) |
69.78 (59.89-78.48) |
99.34 (97.35-99.84) |
33.49 (20.91-48.96) |
Discussion
Histopathology is the gold standard for diagnosis of squamous intraepithelial lesions and invasive carcinoma. However, because of the inter-observer variations, better biomarkers have been used to assist in some cases with equivocal pathologic features.
In the present study, the maximum patients with cervical lesions were in the age group of 40 to 49 years. Chhabra et al[10] also observed that more than two thirds of the women with various cervical lesions were in the reproductive age group, collaborating the fact that sexually active women in the reproductive age group have a higher chance of having an unhealthy cervix. Similarly, in a study conducted by Sharma et al.[11] the mean age of patients with cervical lesions was 40.06 years and maximum cases of squamous cell carcinoma were observed in patients > 50 years of age which is compatible with our findings.
Early marriage and high parity are well established risk factors for cervical carcinoma because of higher chance of exposure to carcinogenic HPV types. We observed 5(100%) cases of carcinoma and 18(58%) cases of CIN occurring in multiparous women. 4(80%) cases of carcinoma and 13(41.9%) cases of CIN had early age of marriage. Similar findings were observed by Sharma et al[11] and Bhukhari et al.[12]
The most common presenting symptom in the present study was discharge per vaginum in both the premalignant 21(61.7%) and 3(60%) malignant cases, followed by abnormal bleeding per vaginum which correlated well with the study by Pradhan B et al[13] and Bukhari et al.[12]
The Pap smear test is considered as an effective screening method to prevent development of cervical cancer. According to the American cancer society (2012), Pap smear test is a routine cancer screening method that should be done every 3 years for women ages 21 to 65 years and women with 30 years and above can consider Pap testing every 5 years if combined with testing for HPV.[14] In the present study, prior abnormal Pap test results were observed in 100% of the malignant cases and 68.4% of pre malignant conditions.
In the present study, high risk HPV was found to be associated with 80% of carcinoma, 50% of CIN III, 37.5% of CIN II and 10.5% of CIN I. In a study by Agoff S. N. et al,[15] 54% of cervical neoplastic lesions show HPV 16 positivity.
In the present study, expression of p16 and ki 67 and their diagnostic accuracy in cervical intraepithelial neoplasia and carcinoma were studied. 6 cases (31.6%) of CIN I, 5 (62.5%) cases of CIN II, 4 of 4 (100%) CIN III and 5 of 5 (100%) carcinoma cases showed ki-67 expression. There was no ki 67 expression in inflammatory lesions. The expression of ki 67 showed a constant increase with increasing severity of disease. Similar observations were also found in various studies conducted by S Srivastava, [16] Ashok Sangwaiya et al,[17] & Kanjana Kanthiya et al. [18]
In the present study, there was no expression of p16 in inflammatory lesions. p16 overexpression was seen in 5 of 19(26.3%) CIN I, 4 of 8,(50%) CIN II, 3 of 4(75%) CIN III and 4 of 5(80%) carcinoma which is similar to study conducted by Srivastava,[16] Klaes et al[19] & Calil LN et al.[20] However, one case of carcinoma showed only weak cytoplasmic staining of p16 which was considered as negative and may indicate that p16 negative carcinomas do exist. Such findings were also observed by Volgareva et al.[21] The probable explanation could be that in these p16 negative cases there is suppression of its upregulation through epigenetic mechanisms, such as promoter methylation or genetic mechanisms such as deletion or loss of heterozygosity.
In the present study, the sensitivity and specificity to detect ≥ CIN II lesions were 76.47% and 91.95% by p16 and 82.35% and 92.4 % by ki 67 and specificity were highest at 97.65% when both the markers were used together. Our findings are concordant with that of Kanjana Kanthiya et al[18] and Van et al.[22]
Conclusion
Most of the cases of premalignant and malignant lesions of the cervix had strong association with HR-HPV. Inflammatory lesions did not take up p16 and ki-67 immunostains. p16 and ki 67 immunoreactivity in premalignant and malignant lesions showed a constant increase with increasing severity of the disease and specificity was highest when both the stains were used together. Hence, it can be concluded that p16 and ki 67 immunoexpression may be used for the diagnosis of cervical premalignant and malignant lesions in conjunction with the histomorphological features to differentiate true dysplasia from reactive changes, thereby increasing the diagnostic accuracy which would have a major impact on treatment.
Source of Funding
No financial support was received for the work within this manuscript.
Conflict of Interest
The authors declare they have no conflict of interest.
References
- Torre L, Bray F, Siegel R, Ferlay J, Tieulent JL, Jemal A. Global cancer statistics. CA: Cancer J Clin. 2015;65(2):87-108. [Google Scholar] [Crossref]
- . World Health Organization, Comprehensive Cervical Cancer Control: A Guide to Essential Practice. 2nd Edn.. 2014. [Google Scholar]
- Arbyn M, Weiderpass E, Bruni L, Sanjosé S, Saraiya M, Ferlay J. Estimates of incidence and mortality of cervical cancer in 2018: a worldwide analysis. Lancet Global Health. 2020;8(2):e191-e203. [Google Scholar] [Crossref]
- Schiffman M, Wentzensen N. From Human Papillomavirus to Cervical Cancer. Obstet Gynecol. 2010;116(1):177-85. [Google Scholar] [Crossref]
- Cuschieri K, Wentzensen N. Human Papillomavirus mRNA and p16 Detection as Biomarkers for the Improved Diagnosis of Cervical Neoplasia. Cancer Epidemiol Biomarkers Prev . 2008;17(10):2536-45. [Google Scholar] [Crossref]
- Tsoumpou I, Arbyn M, Kyrgiou M, Wentzensen N, Koliopoulos G, Martin-Hirsch P. p16INK4a immunostaining in cytological and histological specimens from the uterine cervix: A systematic review and meta-analysis. Cancer Treat Rev . 2009;35(3):210-20. [Google Scholar] [Crossref]
- Wentzensen N, Bergeron C, Cas F, Eschenbach D, Vinokurova S, Doeberitz MK. Evaluation of a nuclear score for p16INK4a-stained cervical squamous cells in liquid-based cytology samples. Cancer. 2005;105(6):461-7. [Google Scholar] [Crossref]
- Darragh TM, Colgan TJ, Cox JT, Heller DS, Henry MR, Luff RD. The lower anogenital terminology standardization project for HPV-associated lesions:background and consensus recommendations from the college of American pathologist and the American society for colposcopy and cervical pathology. Arch Pathol Lab Med. 2012;136(10):1266-97. [Google Scholar]
- Anju M, Madhu G. Assessment of monoclonal antibodyMIB-1labelling indices in cervical intra epithelial lesions of the uterine cervix in paraffin section. J Obstet Gynecol India. 2008;58(4):327-32. [Google Scholar]
- Chhabra Y, Behera BG, K. Cytomorphological study of PAP smears for precancerous and cancerous lesions. J Cytol. 2003;20:64-7. [Google Scholar]
- Sharma A, Singh S. Spectrum of Cervical Lesions and Cytohistological Correlation: A Study in Tertiary Care Center. Int J Contemp Med Res [IJCMR]. 2019;6(6):5-10. [Google Scholar] [Crossref]
- Bukhari M, Qamar S, Niazi S, Saba K, Majeed M, Naeem S. Clinicopathological importance of Papanicolaou smears for the diagnosis of premalignant and malignant lesions of the cervix. J Cytol. 2012;29(1):20-5. [Google Scholar] [Crossref]
- Pradhan B, Pradhan SB, Mital VP. Correlation of PAP smear findings with clinical findings and cervical biopsy. Kathmandu Univ Med J(KUMJ). 2007;5(4):461-7. [Google Scholar]
- Branca M, Ciotti M, Santini D, Bonito LD, CG, Benedetto A, et al. INK4A) expression is related to grade of cin and high-risk human papilloma virus but does not predict virus clearance after conization or disease outcome. Int J Gynecol Pathol. 2004;23(4):354-65. [Google Scholar]
- Agoff SN, Lin P, Morihara J, Mao C, Kiviat NB, Koutsky LA. p16INK4a Expression Correlates with Degree of Cervical Neoplasia: A Comparison with Ki-67 Expression and Detection of High-Risk HPV Types. Modern Pathol. 2003;16(7):666-673. [Google Scholar] [Crossref]
- Srivastava S. MIB-1: An immunohistochemical expression in preneoplasia and neoplasia of the cervix. Indian J Pathol Microbiol. 2010;53(3):518-24. [Google Scholar]
- Sangwaiya A, Gill M, Bairwa S, Chaudhry M, Sen R, Prakashkataria S. Utility of P16/INK4a and Ki-67 in Pre neoplastic and Neoplastic Lesions of Cervix. Iran J Pathol . 2018;13(3):308-16. [Google Scholar]
- Kanthiya K, Khunnarong J, Tangjitgamol S, Puripat N, Tanvanich S. Expression of the p16 and Ki67 in Cervical Squamous Intraepithelial Lesions and Cancer. Asian Pac J Cancer Prev. 2016;17(7):3201-6. [Google Scholar]
- Klaes R, Friedrich T, Spitkovsky D, Ridder R, Rudy W, Petry U. Overexpression of p16INK4A as a specific marker for dysplastic and neoplastic epithelial cells of the cervix uteri. Int J Cancer. 2001;92(2):276-84. [Google Scholar] [Crossref]
- Calil L, Edelweiss M, Meurer L, Igansi C, Bozzetti M. p16INK4a and Ki67 expression in normal, dysplastic and neoplastic uterine cervical epithelium and human papillomavirus (HPV) infection. Pathol - Res Pract. 2014;210(8):482-7. [Google Scholar] [Crossref]
- Volgareva G, Zavalishina L, Andreeva Y, Frank G, Krutikova E, Golovina D. Protein p16 as a marker of dysplastic and neoplastic alterations in cervical epithelial cells. BMC Cancer. 2004;4(1). [Google Scholar] [Crossref]
- Niekerk D, Guillaud M, Matisic J, Benedet J, Freeberg J, Follen M. p16 and MIB1 improve the sensitivity and specificity of the diagnosis of high grade squamous intraepithelial lesions: Methodological issues in a report of 447 biopsies with consensus diagnosis and HPV HCII testing. Gynecologic Oncol. 2007;107(1):S233-40. [Google Scholar] [Crossref]
How to Cite This Article
Vancouver
Devi NK, Devi LS, Singh LR. Expression of P16 and KI-67 in cervical intraepithelial neoplasia and carcinoma: An institute based study [Internet]. IP J Diagn Pathol Oncol. 2021 [cited 2025 Sep 15];6(1):19-24. Available from: https://doi.org/10.18231/j.jdpo.2021.005
APA
Devi, N. K., Devi, L. S., Singh, L. R. (2021). Expression of P16 and KI-67 in cervical intraepithelial neoplasia and carcinoma: An institute based study. IP J Diagn Pathol Oncol, 6(1), 19-24. https://doi.org/10.18231/j.jdpo.2021.005
MLA
Devi, Nongmaithem Karuna, Devi, L. Sushila, Singh, L. Ranjit. "Expression of P16 and KI-67 in cervical intraepithelial neoplasia and carcinoma: An institute based study." IP J Diagn Pathol Oncol, vol. 6, no. 1, 2021, pp. 19-24. https://doi.org/10.18231/j.jdpo.2021.005
Chicago
Devi, N. K., Devi, L. S., Singh, L. R.. "Expression of P16 and KI-67 in cervical intraepithelial neoplasia and carcinoma: An institute based study." IP J Diagn Pathol Oncol 6, no. 1 (2021): 19-24. https://doi.org/10.18231/j.jdpo.2021.005
