Introduction
The clinical laboratory plays an increasingly pivotal role in the patient-care services. Physicians depend on accurate laboratory test results for proper disease diagnosis and for establishment of exact therapy.1 Clinical laboratory errors can reflect on increased healthcare costs and decreased patient satisfaction. Laboratory errors can happen at any of the three stages, studies show that the pre-analytical phase accounts for 46% to 68.2%.2 However, with recent improvements in pre-analytical automation, the pre-analytical phase is still the most error-prone phase in a laboratory.2 Thus, this study is done to identify the different preanalytical errors in the central laboratory and corrective strategies taken to overcome them.
Material and Methods
Current study was a descriptive one and it was carried out in the Central Laboratory, Mahatma Gandhi Medical College and Research Institute, Pondicherry. Duration of study was one year from September 2018 to August 2019. The study included all the samples collected from the Central laboratory, Mahatma Gandhi Medical College and Research Institute, which included departments like Pathology, Biochemistry and Microbiology. The samples were received along with the patients request form which included the necessary and mandatory patients details. The errors in the preanalytical phase were noted as per the ISO 15189: 2012 in a separate register and risk on the patient safety was assessed based on Failure model and effects analysis (FMEA) and categorised into various grades of severity like highly hazardous, hazardous, very high, high, moderate and low.3 Necessary corrective measures were implemented and pre-analytical errors were reassessed. A total of 500 samples were studied in this study period. Amongst 500 samples received, preanalytical errors were detected in 263 samples. The study and data accumulation were carried out with approval from the Institutional Human Ethics Committee. Z-test was applied to compare the results pre and post intervention of corrective measures.
Results
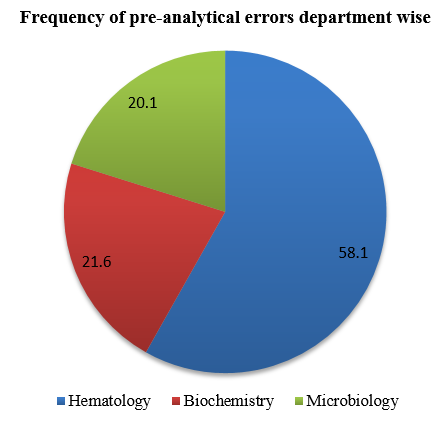
Amongst 263 samples that had pre-analytical errors, Majority 83.6% were from inpatient wards, whereas 16.4% samples were from outpatient departments, 58.1% samples that had pre-analytical errors, were from Hematology, 21.6% samples were from Biochemistry and 20.1% samples were from Microbiology. Refer to Figure 1.for the frequency of pre-analytical errors department wise.
167(63.4 %) samples were blood samples, 89(33.8%) were serum samples and 7(2.6%) were urine samples. The pre-analytical errors detected were Insufficient volume (27.7%), Diluted sample (14.8%), Insufficient information (wrong vial/wrong slip) (14.4%), Mismatch name (8.3%), Clotted sample (15.2%), Lipemic sample (7.2%) and Hemolysed sample (12.16%). The most common pre-analytical error encountered was insufficient volume accounting to 27.7% and least encountered pre-analytical error was Lipemic sample accounting to 7.2%.The causes for the pre-analytical errors were evaluated, and the most common cause was lack of proper technique of phlebotomy by the nurses and phlebotomists, which was overcome by providing necessary training programmes and revision of Standard Operating Protocol(SOP). Table 1: percentage of pre-analytical errors and nature of sample.
Table 1
Percentage of pre-analytical errors and nature of sample
Failure Mode and Effects Analysis (FMEA) was applied to assess the severity of risk of pre-analytical error on patients safety. Out of all the pre-analytical errors, insufficient volume, diluted sample, mismatch name, clotted sample and lipemic sample were graded as very high with scale of 8, as lipemic sample can seriously interfere in patients value interpretation and can also affect in clinical management of the patient. Insufficient information alone was graded as high grade with scale 7. Table 2: severity of risk assessment of pre-analytical errors.
Table 2
Severity of risk assessment of pre-analytical errors
Table 3
Corrective strategies in reducing pre-analytical errors in central laboratory
A total of 500 samples were studied again, after implementation of the above corrective strategies in the laboratory. Amongst 500 samples, 87(17.4%) samples had pre-analytical errors. Out of 87 samples that had pre-analytical errors, 53(60%) samples that had pre-analytical errors, were from inpatient and 34(39%) samples were from out-patient. Refer to table 3: corrective strategies in reducing pre-analytical errors in central laboratory. Z-test was calculated, on comparing the results of pre and post intervention, which showed z=11.6 and p=0.001. Thus, showing statistical significance.
Discussion
In the present study, out of 263 samples that had pre-analytical errors, majority 83.6 % were from inpatient wards and 16.4 % were from outpatient departments. Study conducted by Pavani B et al also showed majority of percentage from inpatient departments. 4 Our study coincides with the above mentioned study. In the present study, out of 263 samples that had pre-analytical errors, 58.1 % were from Hematology, 21.6 % were from Biochemistry and 20.1 % were from Microbiology. This is the only study which included samples from Hematology, Biochemistry and Microbiology. Other studies conducted by Shashi Upreti et al, Shukla et al, Narang et al and Pavani B et al included samples from Hematology, whereas study conducted by Sumera Naz et al included samples from Biochemsitry.4, 5, 6, 7, 8 Out of 263 samples that had pre-analytical errors, 54.3 % samples were blood samples, 42.9% were serum samples and 2.6% were urine samples. Whereas, studies conducted by Shashi Upreti et al, Shukla et al, Narang et al and Pavani B et al involved blood samples, and study conducted by Sumera Naz et al. involved serological samples.4, 5, 6, 7, 8 No study showed pre-analytical errors of urine samples. Our study more or less correlates with the above studies.
In the present study, the most common cause of pre-analytical error in blood and urine samples was insufficient volume, which accounted to 36.3 % and 57.1 %, whereas the most common cause of pre-analytical error in serological samples was hemolysis. which accounted to 28.3 %. Studies conducted by Shukla et al, Narang et al and Sumera Naz et al showed the most common cause of pre-analytical error was clotted sample, whereas study conducted by Pavani B et al showed the most common cause of pre-analytical error was mismatch sample. 4, 5, 6, 7, 8 This is because the nursing staff didn’t draw enough volume of blood and few samples were hemolysed on transportation.
Although, there are many articles on pre-analytical errors and their corrective actions in a laboratory, there are very few articles with risk assessment of safety on patient and implementation of FMEA( Failure model and effects analysis).So, in order to bring such pre-analytical errors under control, regular training programmes for the laboratory technicians and diagnosticians should be implemented as a hospital policy, followed by assessment of the knowledge and skills in the quality management system of laboratory.
Conclusion
Alhough there are lots of development in analytical phase of testing in clinical labs, many errors still occur and they will continue to occur in pre-analytical phase.9 Such pre-enalytical errors can be overcome by better coordination between labs and wards, continuing medical education programmes of laboratory staff, computerization of the labs and competency check of staff. 10