Introduction
Tuberculosis is known to be one of the major cause of morbidity and mortality worldwide. The incidence of extrapulmonary tuberculosis is 10-15%, among which most common sites are lymph nodes, followed by pleura.1 Tuberculosis of oral cavity and oropharynx is rarely seen. Tuberculosis of tonsils in absence of active pulmonary tuberculosis is extremely rare. The incidence of tonsillar tuberculosis was high in prepasteurization era due to ingestion of unpasteurized milk and acquiring mycobacterium bovis infection. Incidence of tonsillar tuberculosis has been reduced with antitubercular drugs and pasteurization of milk. Now a days, there is again increase in tonsillar tuberculosis with the emergence of drug resistance. Tonsillar tuberculosis is classified as primary when lungs are not involved and secondary, when associated pulmonary tuberculosis is found. 2 Here we report a case of primary tonsillar tuberculosis in a patient who presented with history of chronic tonsillitis.
Case Report
A 21- year-old male patient came to otorhinolaryngology department with chief complaints of sore throat, difficulty in swallowing, odynophagia and swelling neck since 4 months. There was no associated history of cold, cough and fever. Past and family history of tuberculosis, diabetes, chronic lung disease and any other chronic disease was not present. Patient was non-alcoholic and there was no history of any medications. General physical examination revealed bilateral swelling over submandibular region. Oral cavity examination showed bilateral enlarged, swollen palatine tonsils with associated erythema of surrounding area. Chest X- ray was normal. Routine laboratory investigations like complete blood count, liver function test and renal function test was with in normal limits. Clinical diagnosis of chronic tonsillitis was made. Pre-operative viral markers for Hepatitis-B, Hepatitis-C and HIV were non-reactive. Bilateral tonsillectomy was done and sent for histopathological examination.
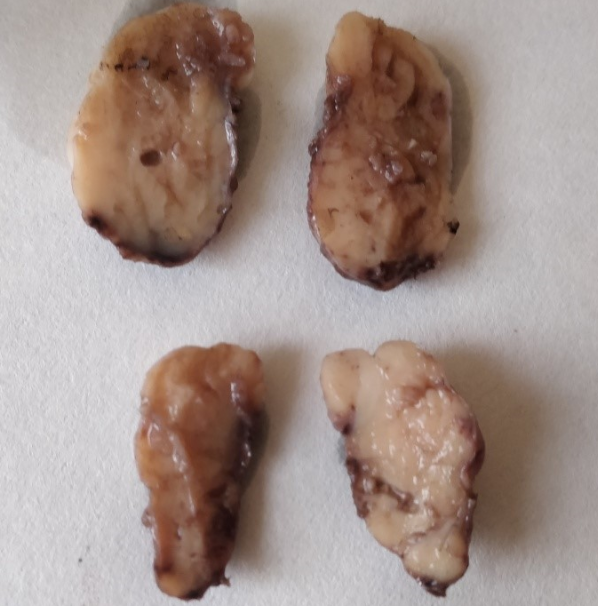
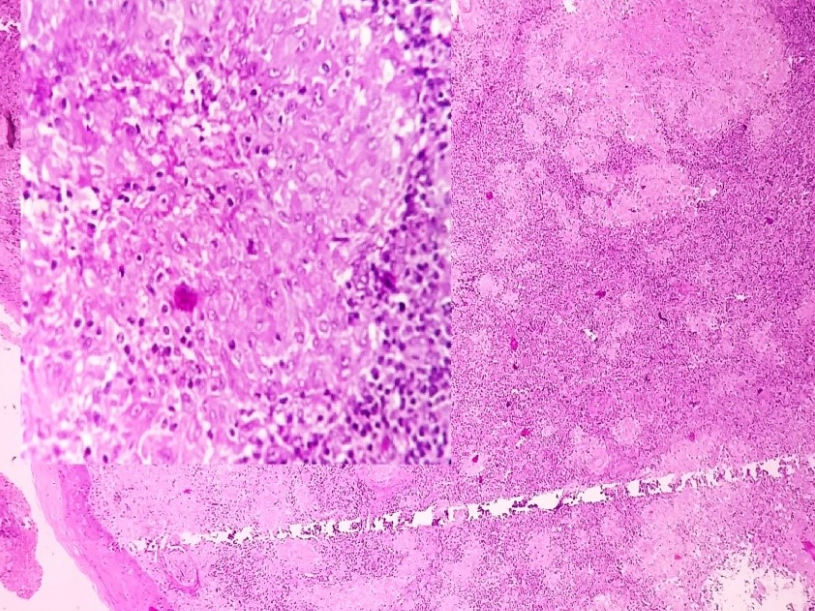
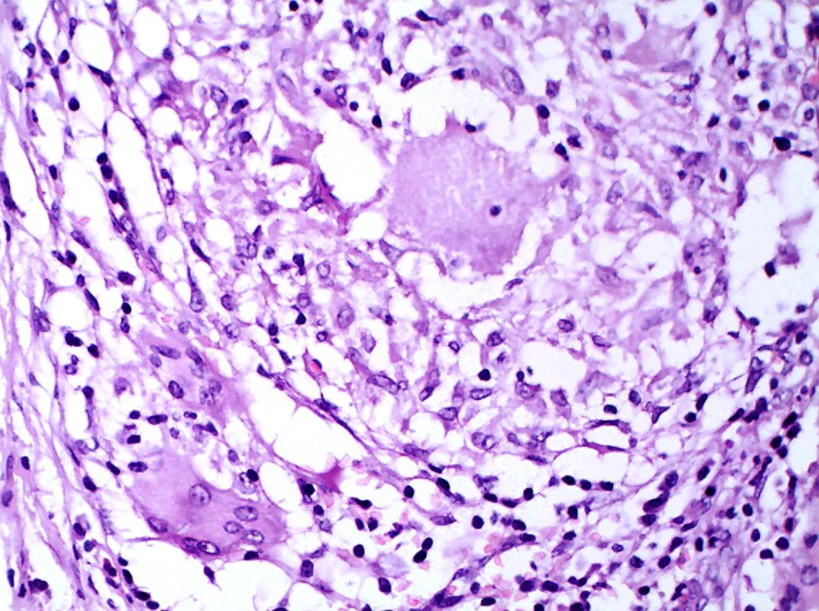
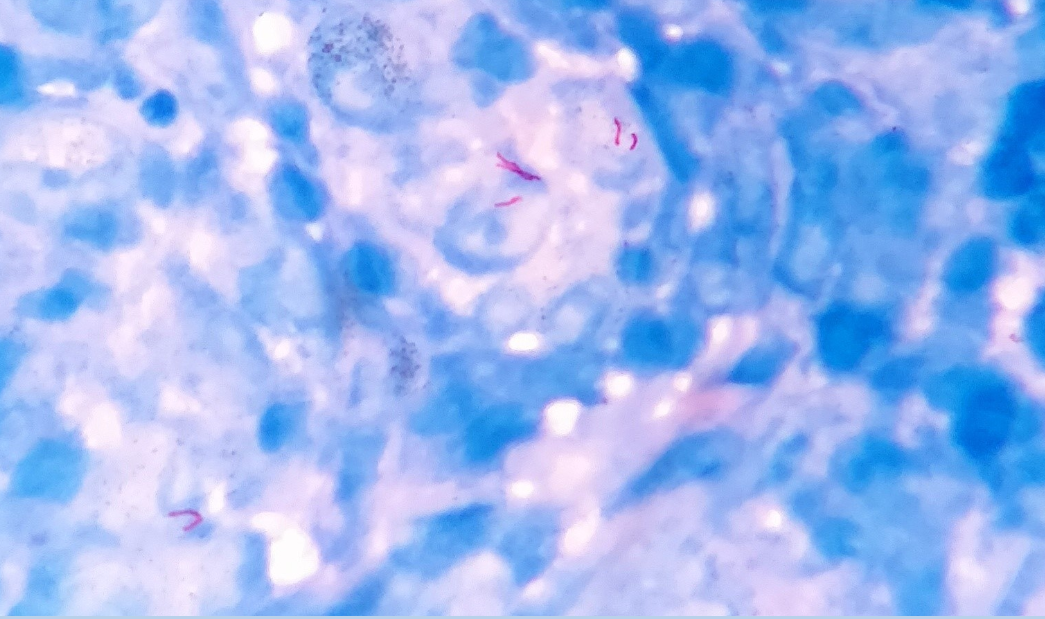
Grossly we received two encapsulated globular grey white tissue pieces. One measuring 3x2.2x1cm and other measuring 3x1.6x1cm. Cut section of both is homogenous and grey white in color. (Figure 1) Microscopic examination from both the palatine tonsil showed stratified squamous epithelial lining. Beneath the epithelium partially effaced tonsillar architecture was seen with presence of well-formed epithelioid cell granulomas comprising of epithelioid cells, central necrosis and Langhans type giant cells. (Figure 2, Figure 3, Figure 4) Acid fast bacilli was detected by Ziehl-Neelsen (ZN) stain. (Figure 5) Thus a diagnosis of Primary Tuberculosis of bilateral palatine tonsils were rendered histopathologically.
Discussion
Approximately 25% of overall tubercular morbidity is due to extrapulmonary involvement. Most common site of extrapulmonary tuberculosis is lymph node tuberculosis while other forms may include pleural tuberculosis, skeletal tuberculosis, CNS tuberculosis, abdominal tuberculosis, genitourinary tuberculosis, miliary tuberculosis and tubercular pericarditis. Tuberculosis of oral cavity is uncommon and tonsillar tuberculosis being rare with an incidence of less than 5%. It can occur due to ingestion of unpasteurized cow’s milk or can result from contact with infected sputum, hematogenous spread and inhalation of tubercle bacilli.3 Irwin Moore classified tonsillar tuberculosis as primary where lungs are not involved and secondary form of tonsillar tuberculosis when sputum positive pulmonary tuberculosis is documented.4
Palatine tonsils are located at a site which is frequently exposed with infected sputum or saliva. Tonsillar tuberculosis is still very rare because of protective stratified squamous epithelium covering, antiseptic role of saliva, presence of saprophytes of oral cavity, and inherent resistance of tonsils to tuberculosis. 5 The various predisposing factors include poor dental hygiene, dental extraction, periodontitis, and leukoplakia. Tonsillar enlargement, sore throat, cervical lymphadenopathy, odynophagia, with or without constitutional symptoms and signs of tuberculosis are the various clinical presentations in case of tonsillar tuberculosis. No age and sex predilection was found in the previous literature.2 Our case presented with enlarged swollen tonsils with chief complaints of sore throat, difficulity in swallowing, odynophagia and swelling neck. No associated constitutional symptoms were present.
Diagnosis of tonsillar tuberculosis is done by histopathology, Ziehl Neelsen staining and mycobacterial culture. Epithelioid granulomas with caseous necrosis, Langhan’s giant cells with or without acid bacilli are features of tonsillar tuberculosis. Sputum smear and chest X-ray should be done to rule out pulmonary involvement. 6 History of chronic alcoholism, long term steroid use, COPD, diabetes, chronic renal failure, pregnancy, and HIV infection should be taken, as tonsillar tuberculosis is more common in patients with poor immunity. Traumatic ulcers, aphthous ulcers, malignancy, wegener's granulomatosis, actinomycosis, chronic tonsillitis should be considered in differential diagnosis. Treatment of tonsillar tuberculosis is antitubercular therapy.3, 7
In conclusion, Tuberculosis is a severe life threatening disease. Primary tuberculosis of tonsils is a rare entity. In developing countries like India where the incidence of tuberculosis is high, the possibility of tonsillar tuberculosis should be considered. Unequally enlarged tonsils, history of sore throat and difficulty in swallowing are clue to diagnosis. Early diagnosis and intervention is essential for cure.