- Visibility 60 Views
- Downloads 9 Downloads
- DOI 10.18231/j.jdpo.2020.039
-
CrossMark
- Citation
Histopathological study of prostatic lesions in a tertiary care hospital
- Author Details:
-
Rupali Yelave
-
Zaidi Shahnaaz
-
Vishrabdha Pawar *
Introduction
Prostate is a glandular and fibromuscular organ located in the retroperitoneum encircling the neck of the urinary bladder. [1] With increasing age most of the other organs undergo atrophy but mostly the prostate undergoes hyperplasia and is of clinical relevance [2] benign lesions usually presents with frequency and nocturia, whereas haematuria and intermittent stream are significantly associated with malignant lesions.[3] Over the age of 50 years BPH is an extremely common condition and shows remarkable racial and geographical variation in incidence and mortality.[4] Among all the countries in Asia prostatic carcinoma is more common in India.[5] Early detection of prostatic malignancy is essential to prevent an equal rise in mortality. This study comprises incidence and occurrence of various prostatic lesions like BPH, prostatitis and carcinomas in prostate, morphological changes, serum PSA level correlation and to grade and score the prostatic carcinomas by application of modified Gleason scoring system.
Aim a nd Objectives o f study
Aim
To study histopathological patterns of prostatic lesions in prostate specimens of the patients admitted in Bharati medical college and hospital, Sangli.
Objectives
To study various histopathological patterns of Prostatic lesions.
To find out the occurrence of Benign Prostatic Hyperplasia, Prostatitis & type of carcinoma Prostate graded on modified Gleason scoring system.
Material and Methods
The study titled “Histopathological Study of Prostatic Lesions In A Tertiary Care Hospital, Sangli” was an observational study conducted in the department of Pathology, Bharati Vidyapeeth Deemed to be University Medical College and Hospital, Sangli in the period of December 2016- June 2018. The IEC no.167- A BV (DU) C&H/SANGLI/IEC 2017-18.
Inclusion criteria
All Prostate Specimens received during study period where included in the study.
Exclusion criteria
Patients not giving consent where excluded from the study.
The clinical history and the details of the patients were collected from requisition form. A careful and detailed gross examination was performed of all the prostatic specimens. The specimens obtained were fixed in 10% formalin for the period of 12-24 hrs and then the specimens were submitted for processing, H & E stained slides were examined under light microscope and the prostatic lesions were categorized as benign and malignant lesions. In case of Carcinoma, Gleason’s (modified) scoring system was applied. Microsoft Word and Excel were used to generate graphs and tables. Results are presented as number and percentage for qualitative data.
Observations & Results
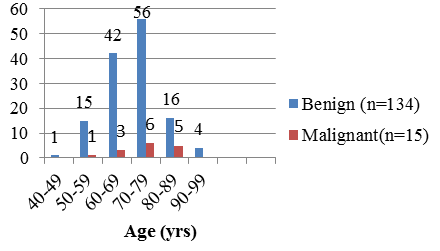
The present study included 149 prostatic specimens. These prostatic specimens obtained, constituted 3.39 % of 4394 total specimens received in the department during the same period TURP was done in 144 cases, needle biopsy was done in 3 cases and total prostatectomy was done in 2 cases.
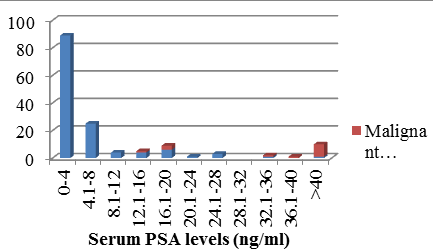
Serum PSA values
Serum PSA levels were done in all the cases. Normal serum PSA levels i.e; 0-4 ng/ml were found in 89/134 case and were all benign. Remaining 45/134 cases showed increase in serum PSA levels due to inflammation, BPH, instrumentation, infarct etc. 9/15 malignant lesions 60% had serum levels more than 40 ng/ml.
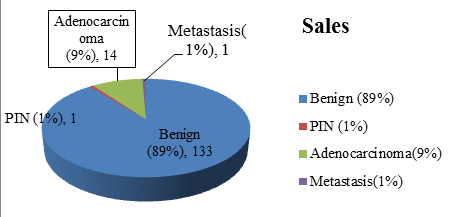
Prostatic lesions
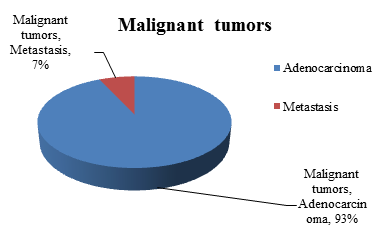
Out of 149 prostatic specimens received, 133 cases were benign lesions, 1 case was PIN, low grade PIN which showed features of epithelial crowding and stratification 14 cases of adenocarcinoma and 1 case of metastasis. Incidence of benign lesions was 89%, PIN lesions was 1% and malignant lesions was 9% and with metastasis was 1%
Benign lesions
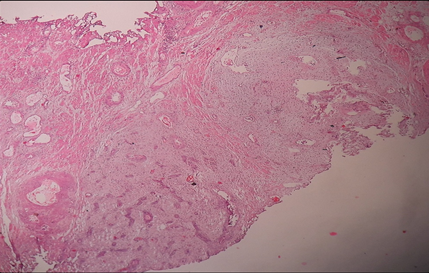
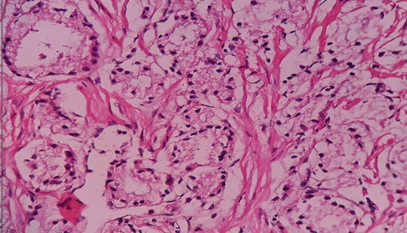
Out of total 133 benign lesions 42 cases were cases of BPH. The lesions were composed of varying proportion of epithelium and stromal hyperplasia. 91 cases were showing BPH with associated findings.
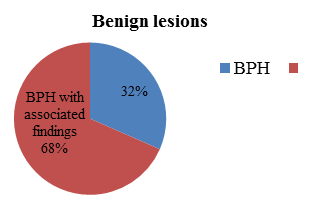
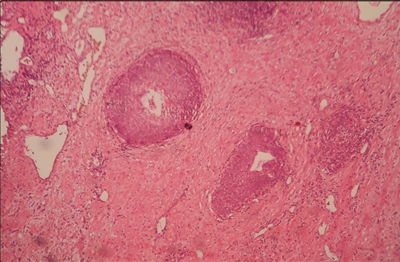
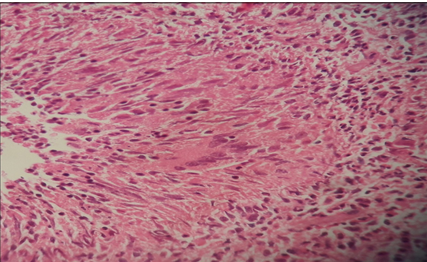
Microscopic features in benign lesion of BPH with associated findings
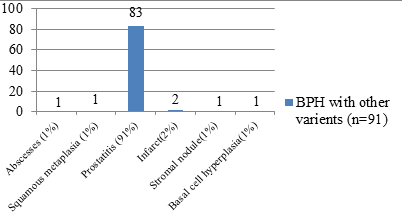
In present study, 91 cases showed benign lesion of BPH with associated findings. 83 cases showed chronic inflammatory cell infiltrate composed of admixture of lymphocytes and plasma cells. 2 cases were showing BPH with granulomatous prostatitis with scattered epitheloid cells, 2 cases showed BPH with infarct and 1 case each of BPH with abscesses, BPH with stromal nodule, BPH with squamous metaplasia and BPH with basal cell hyperplasia.
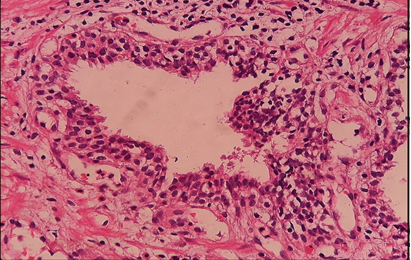
Malignant lesions
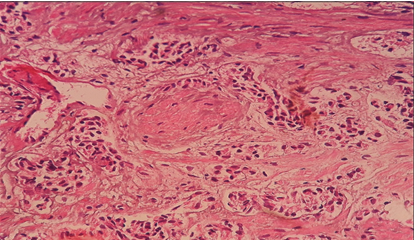
Out of total 15 malignant lesions 14 cases were of adenocarcinoma and 1 case of metastasis.
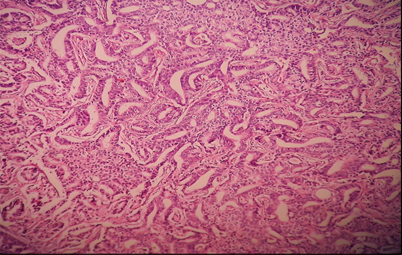
Out of 14 cases of adenocarcinoma 13 were of acinar adenocarcinoma and 1 case of ductal adenocarcinoma. All of them showed one or more of the different growth patterns and were categorized on the predominant growth pattern. Modified gleasons score was given and histopathological grading was done.
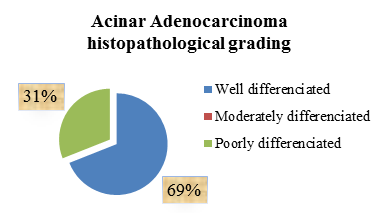
Gleasons score
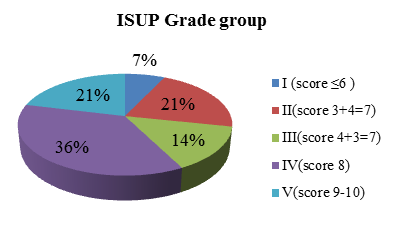
All of these 14 malignant cases were graded using Modified Gleasons scoring system. Modified Gleason score of 7 and 8 was the commonest pattern in 5 cases each (36%). The modified Gleason score of 9 was seen in 3 cases (21%). The modified Gleason score of 6 was seen in 1 case (7%). The earlier pattern of Gleasons score were not seen in the study.
ISUP Grade group
According to the Modified Gleasons score the ISUP grade group was given.

Discussion
The most important histopathological prostatic lesions in the present study are benign prostatic hyperplasia (BPH), BPH with other findings, Prostatic carcinoma and PIN respectively. This study was undertaken to evaluate various histopathological patterns in prostatic lesions and to find out the occurrence of BPH, prostatitis, prostate cancer and to grade these prostatic cancers by application of modified Gleasons scoring system.
Grossly we received 144 TURP specimens out of 149 total specimens consisted of multiple gray tan soft tissue bits weighing ranged from 1-60 grams, 3 needle biopsy which was 2-3 linear soft tissue measuring 1-1.5 cm in length and 2 total Prostatectomy specimen which was nodular with solid and cystic areas on cut surface. Most patients were over the age of 48 years.
The present study showed that majority, 89% (133/149) of cases were benign lesions, of which 32% (42/133) were of benign nodular hyperplasia/ nodular hyperplasia and remaining 68% (91/133) were of BPH with other associated findings. Followed by 1% (1/149) of PIN and 9% (14/149) cases of adenocarcinoma and 1% (1/149) of metastasis.
| Histopathological Diagnosis | Mittal BV et al.5 (1989) | George E et al.6 (2005) | Maru et al (2014)7 | Present study |
| Nodular hyperplasia | 103 (55.67%) | 1029 (88.5%) | 534 (81.53%) | 42 (28.18%) |
| Prostatitis | 30 (16.24%) | - | - | 83 (55.70%) |
| Granulomatous prostatitis | 3 (1.62%) | - | 02 (0.30 %) | 02 (1.35%) |
| Basal cell hyperplasia | 10 (5.4%) | - | 01 (0.67%) | |
| Metaplasia | 19 (10.27%) | - | - | 01 (0.67%) |
| Atypical adenomatous hyperplasia | 04 (2.16%) | - | - | - |
| Atrophy | 03 (1.62%) | - | - | |
| Stromal nodule | - | - | 01 (0.67%) | |
| Infarct | - | - | 02 (1.35%) | |
| Abscesses | - | - | 01 (0.67%) | |
| PIN | - | 7 (0.6%) | 72 (10.99%) | 01 (0.67%) |
| Carcinoma | 13 (7.02%) | 127 (10.9%) | 47 (7.17%) | 15 (10.07%) |
| Total no of prostatic specimens | 185 | 1163 | 655 | 149 (100%) |
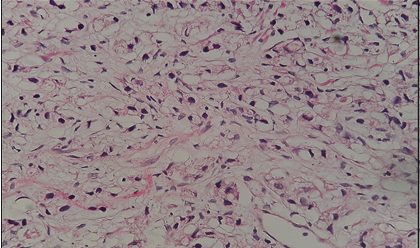
In present study out of 149 cases, 86 cases were of prostatitis. In the study of Shukla P et al[8] 22 cases of granulomatous prostatitis were found with incidence of 1.86%. BPH with Chronic nonspecific Prostatitis was seen in 83/86(96.55%) and BPH with abscesses was seen in 01/86 (1.16%) in 55 years. In the present study 2 cases showed BPH with granulomatous prostatitis in the age group of 75 and 77 respectively. The serum PSA was 5.5ng/ml and 8 ng/ml. No evidence of caseation was seen and special stain was done for AFB which was negative. In a study of Stillwell et al[9] total 200 cases of granulomatous prostatitis were reported In study by Granados et al[10] 25 cases of prostatic abscesses showed sheets of neutrophils in and around the acini. In the study of Mohan H et al [11] 20 cases of granulomatous prostatitis was found 12 cases of nonspecific granulomatous prostatitis.
In the present study out of 149 cases 1 case showed PIN which was Low grade prostatic intraepithelial neoplasm and this low grade prostatic intraepithelial neoplasm was seen in age of 85 years which was characterized by epithelial crowding and stratification. In the study by McNeal and Bostwick frequency of PIN was highest in the age group of 60-69 years with mean age of 65 yrs.[12]
In present study peak incidence of prostatic carcinoma was seen in age group of 61-80 yrs which is similar to the findings of other studies.
| S. No | Authors | Study period | Prostate specimens | Prostatic carcinoma | Prevalence |
| 1 | Garg et al(2013) 17 | 18 months | 364 | 79 | 21.70 |
| 2 | Aslam et al(2013) 13 | 3yrs | 48 | 06 | 12.5 |
| 3 | Albasri et al (2014) 14 | 8yrs | 417 | 74 | 17.74 |
| 4 | Begum et al (2015) 15 | 19 months | 50 | 2 | 4 |
| 5 | Hirachand S et al (2017) 16 | 2 yrs | 128 | 13 | 10.15 |
| 6 | Present study | 12 months | 149 | 15 | 10.06 |
Comparative incidence of carcinoma with reference to Gleason`s score
Atchyuta et al (2016) [18] reported the distribution of Gleason`s score in 75 cases of prostatic carcinoma. Also, Varma et al (2002) [19] reported the distribution of Gleason`s score in 150 malignant i.e cases of prostatic carcinoma. Anushree C.N et al, (2012) [20] reported the distribution of Gleason`s score in 12 cases of prostatic carcinoma.
And in the present study the distribution was done according to the modified Gleason`s score in 14 cases out of 15 malignant cases as 1 was of metastasis. After the gleasons score the ISUP grading was also done in this study.
Normal levels of PSA are usually 0-4 ng/ml but they vary according to the age of the patient. PSA density- Serum PSA density reflects the PSA produced per gram of prostatic tissue. PSA density is calculated by dividing the total serum PSA level by estimated gland volume (usually determined by TRUS measurements) with upper normal value of approximately 0.15. [21]
Age specific reference range [21]
Men of 40- 49years – The age specific upper reference ranges for Serum PSA are 2.5 ng/ml.
Men of 50- 59years – The age specific upper reference ranges for Serum PSA are 3.5 ng/ml
Men of 60- 69years – The age specific upper reference ranges for Serum PSA are 4.5 ng/ml
Men of 70- 79years – The age specific upper reference ranges for Serum PSA are 6.5 ng/ml
In the present study, serum PSA was done in all the cases. Out of 149 cases 134 were benign from which 89 cases had normal PSA levels and all were benign but the remaining 45 cases of benign lesions showed increase in serum PSA levels. 6 cases showed elevation more than 20ng/ml in benign cases. The rise in serum PSA was not only due to malignancy but also due to the prostatic manipulations including cystoscopy, needle biopsy, and also due to other benign lesions like prostatitis, abscesses, infarct, granulomatous prostatitis etc. In all malignant lesions serum PSA was significantly raised above normal limits. 9/15 malignant lesions 60% had serum levels more than 40 ng/ml.
Summary
This study entitled “Histopathological Study of Prostatic Lesions in A Tertiary Care Hospital,” was conducted with the aim to study histopathological patterns of prostatic lesions in prostate specimens of the patients admitted in hospital, with following objectives-
To study various histopathological patterns of prostatic lesions.
To find out the occurrence of Benign Prostatic Hyperplasia, Prostatitis & type of carcinoma prostate graded on modified Gleason scoring system.
This study was conducted from December 2016- June 2018. Only the patients not willing for the consent where excluded from the study.
A total of 149 cases were studied. Out of these TURP was done in 144 cases (97%), Needle biopsy in 3 cases (2%) and total prostatectomy in 2 cases (1%). The commonest pathology encountered was benign lesions i.e 133 cases (89%), 1 case (1%) of PIN and 14 cases (9%) of adenocarcinoma of prostate and 1 case (1%) of metastasis. Among 133 cases 42 cases (32%) were of BPH and remaining 91 cases (68%) had BPH with other associated findings
Out of 149 total cases. 15 cases (10.06%) were having malignant lesions 13 cases of acinar adenocarcinoma, 1 with ductal adenocarcinoma and 1 with metastasis. Common age group of lesions was 70-79 years with commonest symptoms of frequency, urgency and acute retention of urine. Serum PSA levels in 89/134 cases were normal i.e 0-4 ng/ml. Remaining 45/134 cases showed increase in serum PSA levels due to inflammation, BPH, instrumentation or infarcts etc.
15 malignant lesions were common in age group of 70-79 years. Serum PSA was significantly raised in all malignant lesion. 60% of the malignant lesions showed increase in serum PSA levels above 40 ng/ml.
According to the modified Gleasons scoring system and ISUP grading system was done 14 cases out of 15 malignant cases as 1 was of metastasis. Most of these cases had Gleason score of 7 and 8 and the most commonly these lesions fall into ISUP grade group of IV, V and II respectively.
Like most of the other studies done, in our study too we found predominantly benign lesions like BPH & Prostatitis; followed by cases of prostatic adenocarcinomas including a case of metastasis.
Conclusion
Benign prostatic hyperplasia (BPH) with other benign lesions and adenocarcinoma are most common diseases encountered in the present study. Considering the age of the patient and clinical symptoms of lower urinary tract, further examination and investigations like P/R digital examination, ultrasonographic study and serum PSA levels should be done. According to the condition of the patient and the further needle biopsy or TURP can be performed. Interpretation of prostatic biopsy is been challenging to the pathologist because of the mimickers of the carcinoma.
Histopathological study of the prostatic lesions plays an important role in diagnosis, treatment and prognosis of the patient.
For early diagnosis, treatment and for reducing mortality and morbidity immunohistochemistry and molecular genetic analysis should be done along with this screening protocols and awareness programs should to be carried out.
Source of Funding
None.
Conflict of Interest
None.
References
- S Standring. Gray`s Anatomy The Anatomical Basis of clinical Practice. . [Google Scholar]
- A U Hassan, G Hassan, Z Rasool, Zubeida. Aim and Objectives of Histological Studies of Prostate. Universal J Clin Med 2013. [Google Scholar]
- M G Kohale, N Kulkarni, S N Kulkarni, J Surwade. Clinical spectrum of prostatic lesions: A clinicopathological study. 2016. [Google Scholar]
- P C Walsh, PC Walsh, RF Gittes, AD Perlmatter, TA Stamey. Benign prostatic hyperplasia. 1986. [Google Scholar]
- B V Mittal, M B Amin, S G Kinare. Spectrum of histological lesions in 185 consecutive prostatic specimens. J Postgrad Med 1989. [Google Scholar]
- E George, S Thomas. Histopathologic survey of prostate disease in the Sultanate of Oman. Internet J Pathol 2005. [Google Scholar]
- A M Maru, H M Makwana, N R Lakum, T Chokshi, N Trivedi, J Joshi. Study On Correlation Between Prostate Specific Antigen (PSA)And Various Prostatic Pathology. Int J Med Sci Public Health 2014. [Google Scholar]
- Prakriti Shukla, Hanni V. Gulwani, Sukhpreet Kaur. Granulomatous prostatitis: clinical and histomorphologic survey of the disease in a tertiary care hospital. Prostate Int 2017. [Google Scholar]
- Thomas J. Stillwell, Donald E. Engen, George M. Farrow. The Clinical Spectrum of Granulomatous Prostatitis: A Report of 200 Cases. J Urol 1987. [Google Scholar]
- Edgar A. Granados, George Riley, Jose Salvador, Jose Vicente. Prostatic Abscess: Diagnosis and Treatment. J Urol 1992. [Google Scholar]
- H Mohan, A Bal, RP Punia, SA Bawa. Granulomatous prostatitis - an infrequent diagnosis. Int J Urol 2005. [Google Scholar]
- John E. McNeal, David G. Bostwick. Intraductal dysplasia: A premalignant lesion of the prostate. Human Pathol 1986. [Google Scholar]
- Hafiz Aslam, Nazish Shahid, Naseem Shaikh, Hiba Shaikh, Shafaq Saleem, Anum Mughal. Spectrum of prostatic lesions. Int Arch Med 2013. [Google Scholar]
- Abdulkader Albasri, Abeer El-Siddig, Akbar Hussainy, Mervat Mahrous, Abdulaziz Abdullah Alhosaini, Ahmed Alhujaily. Histopathologic Characterization of Prostate Diseases in Madinah, Saudi Arabia. Asian Pacific J Cancer Prev 2014. [Google Scholar]
- Zeenath Begum, Abdul Hakeem Attar, Mandakini B. Tengli, Mohammed Mateen Ahmed. Study of Various Histopathological Patterns in Turp Specimens and Incidental Detection of Carcinoma Prostate. Indian J Pathol Oncol 2015. [Google Scholar]
- S Hirachand, UMS Dangol, S Pradhanang, S Acharya. Study of prostatic pathology and its correlation with prostate specific antigen level. J Pathol Nepal 2017. [Google Scholar]
- Monika Garg, Gurmeen Kaur, Vineeta Malhotra, Ravish Garg. Histopathological spectrum of 364 prostatic specimens including immunohistochemistry with special reference to grey zone lesions. Prostate Int 2013. [Google Scholar]
- M Atchyuta, P Krishna, P P Latha, I V Renuka, V Tejaswini, G Vahini. Histopathological spectrum of prostatic adenocarcinoma in correlation with PSA Values. Indian J Pathol Oncol 2016. [Google Scholar]
- Varma Murali, M W Lee, P Tamboli, R J Zarbo, R E Jimenez, Pgo Salles, M B Amin. Morphologic Criteria for the diagnosis of Prostatic Adenocarcinoma in Needle Biopsy Specimens. A Study of 250 Consecutive Cases in a Routine Surgical Pathology Practice. Arch Pathol Lab Med 2002. [Google Scholar]
- C N Anushree, K Venkatesh. Morphological Spectrum of Prostatic lesions- A Clinicopathological Study. Med Innov 2012. [Google Scholar]
- Jonathan I Epstein, G J Netto. Clinical correlation with biopsy: serum Prostate specific antigen, digital rectal examination, and imaging technique. Biopsy interpretation of the prostate. 2008. [Google Scholar]
- Introduction
- Aim a nd Objectives o f study
- Material and Methods
- Observations & Results
- Serum PSA values
- Prostatic lesions
- Benign lesions
- Microscopic features in benign lesion of BPH with associated findings
- Malignant lesions
- Gleasons score
- ISUP Grade group
- Discussion
- Comparative incidence of carcinoma with reference to Gleason`s score
- Age specific reference range [21]
- Summary
- Conclusion
- Source of Funding
- Conflict of Interest
