Introduction
Histoplasmosis is a non – contagious systemic infection which is caused by a dimorphic fungal organism, Histoplasma capsulatum.1 It is endemic in many parts of the world such as American Midwest, Latin America and Southern Africa.2 In India, West Bengal accounts for the maximum number of cases of histoplasmosis followed by Uttar Pradesh and Delhi.3 The spores of histoplasma capsulatum are inhaled through the respiratory tract and upon reaching the alveoli they get converted into the yeast form and reach the lymphatics via macrophages. Depending upon the immune status of the host, hematogenous dissemination may occur.2 Clinically it has been categorized as primary acute pulmonary form, chronic pulmonary form and disseminated form, with manifestati ons such as weakness, fever, weight loss, mucocutaneous lesions and hepatosplenomegaly.4 About 99% cases are restricted to the lungs and self limiting.2 It mostly affects the immunocompromised patients having tuberculosis and AIDS, but may affect the immunocompetent individuals as well.5
We hereby report a series of four case s of histoplasmosis and aim to emphasize the usefulness of FNA C in the cytodiagnosis of such lesions.
Case Presentation
Case 1
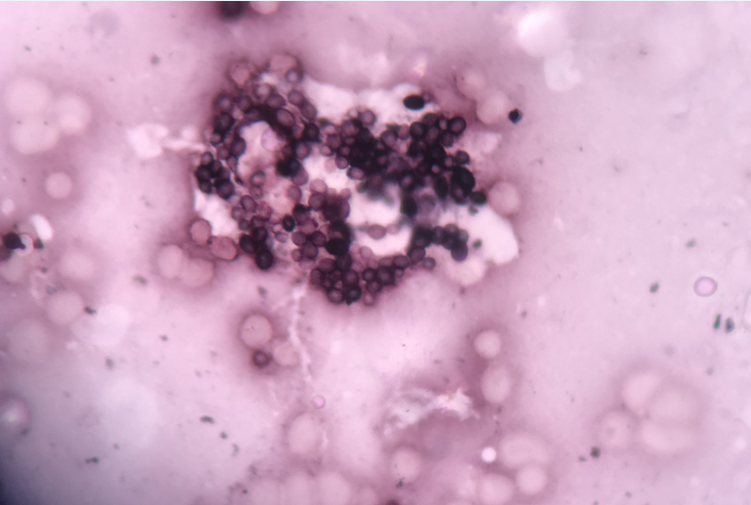
A female patient, aged 50 years, presented in the ENT OPD with the complains of pain and diffuse swelling over the left parotid area for 1 week. She was then referred to the Department of Pathology for FNAC of that diffuse swelling. A detailed history was taken which revealed a dental extraction procedure of left first molar a month ago. There was no history of trauma to the region, chronic cough, weakness, fever, and diabetes mellitus. There was no history of anti tubercular therapy taken or tuberculosis in any of the family members. On examination, a swelling was noted in the left parotid area which was diffuse (approximately 2 X3 cm), soft in consistency, mobile and tender. On general examination, there was no pallor, no lyphadenopathy, no mucocutaneous lesions, and no hepatosplenomegaly. Her haemoglobin was 11.8g/dl, total leucocyte count was 8900/cumm, platelets were 2.90 lacs/mm and peripheral smear showed normocytic normochromic red blood cells with mild anisocytosis. After taking consent from the patient, FNA of the swelling was performed. The smears were stained with May Grunwald Giemsa (MGG) stain and were examined. The smears revealed acinar tissue with a few scattered acute and chronic inflammatory cells along with numerous intracellular and extracellular small rounded organisms with a clear halo around them, morphologically consistent with Histoplasma capsulatum. (Figure 1) The remaining unstained slides were stained with Gomori Methamine Silver (GMS) stain and Periodic Acid Schiff (PAS) stain to study the morphology of the fungal organisms. They were found to be positive for Histoplasma. A workup was done to check the immune status of the patient. Viral markers like HIV, HCV, HBsAg were negative. Her chest X- Ray was done which was normal. Her blood sugar, fasting and post prandial, was also within normal limits. There was no history of alcoholism or immunosuppressant therapy taken so far. She was prescribed oral NSAIDS for 7 days since it was a focal infection and is self limiting in immunocompetent individuals. On follow up, patient responded to the treatment very well.
Case 2
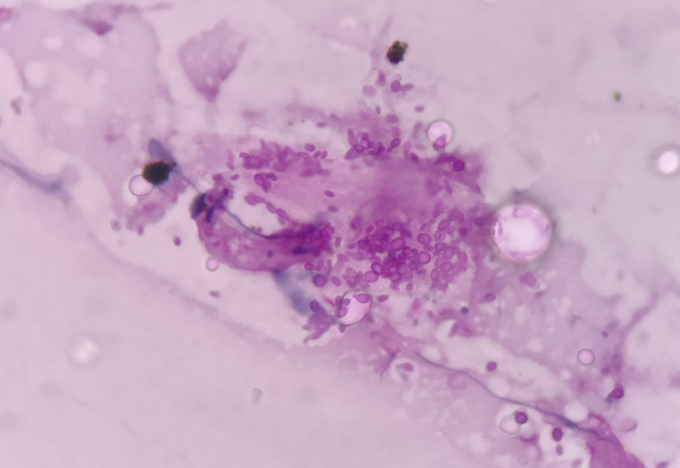
51 year old male patient presented with left submandibular lymph node enlargement since 3 months. The swelling was 2*2 cm in size, mobile, firm and non tender. FNAC was performed after taking informed consent from the patient. The cytology revealed encapsulated organisms within the cystic macrophages in a necrotic background morphologically consistent with Histoplasma capsulatum (Figure 2). GMS and PAS stains were applied to the remaining slide s and were found to be positive. The patient had no complains of chronic cough, fever, weakness, any other swellings or skin lesions. He had no history of chronic alcoholism, diabetes, hypertension, chronic intake of any medications. His hemoglobin was 13.8g/dl, total leucocytes and platelets were within normal limits, his general examination was normal. On further workup of the patient, he was found to have an immunocompetent status with all viral markers negative.
Case 3
A 49 year male patient presented with off and on fever, bilateral cervical lymphadenopathy and molluscum contagiosum like umbilicated lesions all over the face (Figure 3). The general examination revealed no pallor, no icterus and no organomegaly. His hemoglobin was 8.2g/dl, total leucocyte count was 4100 cells/ cumm, platelets were 1.10 per cumm. The patient was a known case of HIV on treatment from 3 months. He had no history of diabetes, hypertension and chronic alcoholism. Other viral markers like HCV and Hbs Ag were negative. His chest X- ray was normal. FNAC was performed from skin lesions and bilateral cervical lymph nodes which revealed numerous encapsulated small round to oval organisms within and outside the histiocytes with granulomas in a necrotic background. The organisms were morphologically consistent with H. capsulatum. GMS and PAS stains were positive for Histoplasma. He was a case of disseminated histoplasmosis with immunocompromised status. The patient was started with oral amphoterecin and was kept under follow up.
Case 4
A 28 year male patient presented with left axillary lymphadenopathy from three weeks. He had no complains of fever, weakness, chronic cough, trauma or tuberculosis in the family. The general examination revealed no pallor, no icterus, no cervical lymphadenopathy, no skin lesions and no organomegaly. Hemoglobin was 14.2 g/dl, total leucocyte count was 9500 per cumm and platelets were 3.10 per cumm. The general blood picture showed normocytic normochromic red blood cells. Chest X-ray was normal. FNAC from the left axillary lymph node revealed encapsulated yeast like organisms packed within the histiocytes. There were no granulomas and no necrosis. The patient’s immune status was evaluated. There was no history of diabetes, hypertension, chronic alcoholism or intake of any immunosuppressant therapy. Serological markers like HCV, HIV and HbsAg were negative. This was a case of isolated histoplasmosis of axillary lymph node.
The cytomorphology was further well delineated by the application of PAS and GMS stains. On GMS staining, the black colored yeast like forms were easily made out having thin pseudo capsule and narrow neck budding against the green background. These features were morphologically consistent with H.capsulatum (Figure 4,Figure 5).
Figure 1
Smear from parotid gland aspirate showing acinar tisssue with a few scattered acute and chronic inflammatory cells along with numerous intracellular and extracellular small rounded organisms with a clear halo around them, morphologically consistent with Histoplasma capsulatum. (MGG stain, 400X)
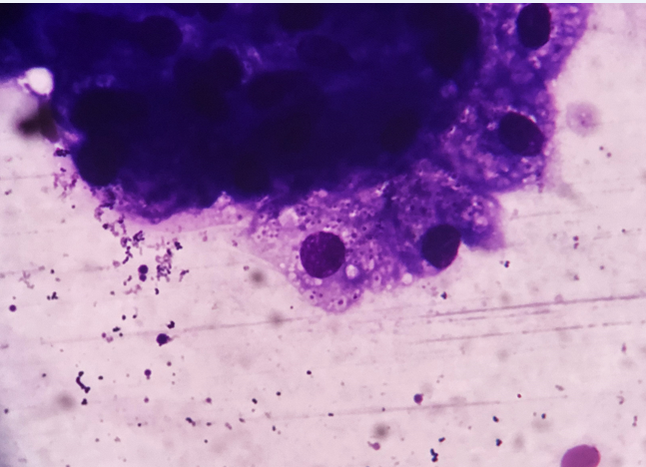
Figure 2
Punched out “holes” in the cytoplasm of a macrophage and in the background representing 3-5 micron yeasts of Histoplasma capsulatum (MGG stain, 1000X)
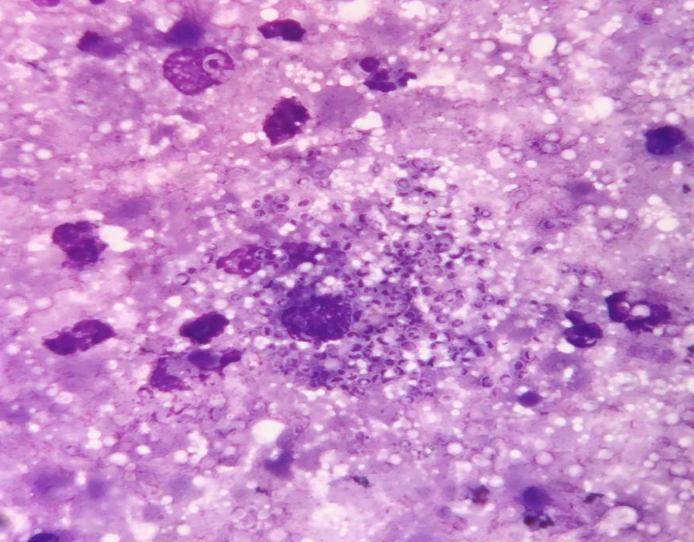
Figure 3
Multiple subcutaneous nodules over the face in an immunocompromised patient diagnosed as Disseminated Histoplasmosis.

Discussion
Histoplasmosis is a sporadic infection in India, with a few states having endemicity namely West Bengal, Uttar Pradesh and Delhi. In India, the first case of histoplasmosis was reported in 1954 by Panja and Sen, in Kolkata.6 Randhawa HS et al, reported 388 cases of histoplasmosis in the Indian subcontinent from 1995 till 2018 and observed a sharp rising trend in the occurrence of this opportunistic infection in recent years.1 On the basis of phenotype, histoplasma is divided into three types- Histoplasma capsulatum var. capsulatum, Histoplasma capsulatum var. duboisii and Histoplasma capsulatum var. farciminosum. The infected birds and bats by their excreta contaminate the soil, which provides the temperature of 22- 29 degree celsius and relative humidity of 67-97% that are optimu m for the growth of microconidia of Histoplasma. The aerolization of these microconidia causes infection.7 These organisms appear as “ punched out holes” or globular to ovoid structures surrounded by a halo on FNAC smears and biopsy specimens. Their characteristic morphology is well delineated by using special stains like GMS and PAS which helps to identify the thin membrane of H. capsulatum that are usually found scattered singly and in clusters.8 However, culture is considered the gold standard diagnostic test for H. capsulatum, but is time consuming, and takes around 2-3 weeks to provide conclusive results.9 PCR can overcome these limitations with definitive results but due to poor resource availability in India, it is not always the best option.1 Kathuria S et al in their analysis done on 61 reported cases of histoplasmosis in immunocompetent patients all over India, showed that maximum number cases were from Uttar Pradesh and West Bengal. They also reported that among these disseminated cases of histoplasmosis in immunocom petent patients, adrenal gland(55.7%) was the most commonly affected site, followed by liver(36%), skin and mucosa(36%), spleen(32.7), lymph nodes(27.8%), lung(18%), pharynx(8.1%).10 Parotid gland involvement by histoplasma capsulatum is extremely rare and have been reported in the literature only in immunocompromised patients or in immunocompetent patients having disseminated disease status. Cases of focal histoplasmosis in immunocompetent individuals are slowly increasing especially among low socio-economic areas which are explained by the sharp rising trend in the disease occurrence in recent years. The common differential diagnosis that enters on the basis of cytomorphology are Leishmania donovani (small intracellular protozoa with a kinetoplast), Cryptococcus neoformans (tear drop shaped spores with mucopolysaccharide rich wide capsule), Coccidioidomycosis immitis (thick walled spores with granular cytoplasm) and Candida (budding yeast cells, pseudohyphae, rarely occurs intracellularly) . These can be ruled out by observing the characteristic morphology of yeast forms of H. capsulatum on GMS and PAS stains.1,11,12 Treatment options include medications like amphoterecin B and itraconazole or fluconazole as induction and maintenance therapy, respectively and follow up of the patient.8
Conclusion
Histoplasmosis is a rare, non endemic opportunistic infection in India which can affect both immunocompromised and immunocompetent individuals. Disseminated histoplasmosis, if not treated can be fatal, therefore it is important to timely diagnose the disease and treat with adequate antifungaldrugs. FNAC of these lesions can be a promising modality for establishing a rapid and confirmatory diagnosis of histoplasmosis and thereby planning early treatment of the disease and avoid unnecessary surgery.