Introduction
Skin, subcutaneous and soft tissues lesions are clinically non- distinctive, forming a varied and complex group showing wide range of differentiation and morphological features. Clinically these lesions are often misdiagnosed due to wide variety of types and their variants.1 There are various conditions which can affect the skin ranging from non-specific dermatoses, inflammatory lesions to neoplastic changes. Adnexal tumors form a varied group of tumors arising from the skin appendages such as sweat glands, sebaceous glands and hair follicles. Soft tissue masses are also frequently encountered lesions with wide range of diagnosis. Fine needle aspiration cytology (FNAC) is a rapid, simple investigative method used to diagnose nodules, superficial and deep-seated soft tissue masses as well as induration and thickening of skin. However, as they are accessible and easily amenable to surgical excision, there is limited application of FNAC in diagnosing these lesions.2 FNAC gains its place in clinician protocol as it is of great help in early timely diagnosis of unusual skin, adnexal and soft tissue masses. It helps in classifying the lesions whether inflammatory, benign or malignant and is also of great utility in differentiating a reactive process which is likely to respond to conservative treatment from a neoplastic process.3
Keeping this in mind a seven years’ retrospective study was done in a teaching medical college with attached hospital in South Delhi to examine the spectrum and cytomorphological features of skin, adnexal and soft tissue lesions by FNAC in patients presenting with lump, nodule or any induration.
Materials and Methods
This was a seven years’ retrospective study from January 2012 to December 2018 conducted in a tertiary care hospital of South Delhi catering to low socioeconomic semi urban population.
Inclusion criteria
All palpable or visible lesions of the skin, subcutis and soft tissues referred by the treating physicians or surgeons for FNAC were included in the study.
Exclusion criteria
Deeper lumps, any nodal, salivary gland lesions were not included in our study.
A total of 15,533 FNAC cases in seven years were received in the cytopathology section out of which 1162(7.5%) were FNACs from skin, adnexa and soft tissues and were included in our study. After taking consent, detailed clinical history of patients along with local examination was done and all radiological and other relevant investigations were studied. Taking all aseptic precautions FNAC was performed using 22 to 24 gauze needles with 10 ml plastic syringe with detachable syringe holder (Franzen Handle). Repeat aspiration was done, wherever needed. Smears were prepared and air dried or wet fixed in 90% ethanol. Air dried smears were stained with MGG and wet fixed were stained with H&E stain. Special stains were performed, wherever necessary. The stained smears were studied and categorized broadly into non neoplastic inflammatory and cystic lesions, neoplastic benign lesions and neoplastic malignant lesions based on the cytomorphology of the lesions. These cases were also subcategorized on the basis of age, sex and location.
Results
Out of a total of 1162 cases of skin, adnexal and soft tissue lesions, non- neoplastic lesions comprised of 447 cases (38.4%). Among the 715 neoplastic lesions, 686 cases (96 %) were benign in nature and rest of the cases were malignancy. 29 cases (4 %). (Table 1) Male to female ratio in non neoplastic, neoplastic-benign and neoplastic- malignant category was. 1:1, 1.5:1, 1.9:1 respectively. (Table 2). Most of the lesions were seen in upper extremities and axilla (27.7%) followed by head and neck region (22.5%). (Table 3) Most frequent non -neoplastic lesion in our study was Epidermal Inclusion Cyst, (45.4%). The second most common lesion was ganglion (14.9%) (Figure 1A,B) followed by Acute Suppurative lesion (14.8%) and Benign Cystic lesion (9.4%). Other lesions commonly reported in our study was Granulomatous lesion (7.2%). (Table 4). We also encountered few rare cases such as two cases of Calcinosis cutis (0.5%) (Figure 2 A,B) and single case each of Herpes Zoster (0.2%) and Scar endometriosis (0.2%). From a total of 447 non neoplastic cases, cytohistological correlation was possible in 198 cases. Out of the 203 cases of epidermal cyst on FNAC, histopathological diagnosis was obtained in 128 cases; which showed good correlation (89%). Lipoma was the most common lesion amongst all neoplastic benign lesions (80.5%) followed by benign mesenchymal lesion (8.5%). (Table 5). Also we encountered rare cases of Pilomatrixoma (0.6%) (Figure 3 A, B), two cases of Infantile Fibromatosis Colli (0.3%), one case each of Granular cell tumor (0.2%) (Figure 4A,B). Histopathological diagnosis was obtained in 285 out of 552 cases of lipomas; 274 cases showed good correlation. (96%) Malignant lesions most commonly seen in our study were metastasis from squamous cell carcinoma (51.7%) followed by adenocarcinoma (20.7%). (Table 6). Two cases of malignant mesenchymal spindle cell tumor (6.9%) were also seen, one on histopathology turned out to be Rhabdomyosarcoma while histopathology was not available in the other case. (Figure 5A,B). One case of malignant melanoma was reported on FNAC which was later confirmed on histopathology. (Figure 6A,B).
Table 1
| Type of Masses | Male | Female | Male: Female Ratio | Total |
| Non-Neoplastic | 238 | 209 | 1.1:1 | 447 |
| Neoplastic-Benign | 414 | 272 | 1.5:1 | 686 |
| Neoplastic- Malignant | 19 | 10 | 1.9:1 | 29 |
| Total | 671 | 491 | 1.4:1 | 1162 |
Cytological spectrum of cutaneous and subcutaneous lesions
Table 2
Age and Sex distribution of Lesions
Table 3
Distribution of cases according to Location
Table 4
Cytologic spectrum of Non neoplastic Lesions (Inflammatory and Cystic lesions)
Table 5
Cytologic spectrum of Neoplastic- Benign Lesions
Table 6
Cytologic spectrum of Neoplastic- Malignant Lesions
Figure 1
(A): Clinical image of Ganglion presenting as wrist swelling; B) Cytosmear from Ganglion Cyst showing histiocyte -like cells with abundant cytoplasm and small oval nuclei in a myxoid background. (H&E, 40x).
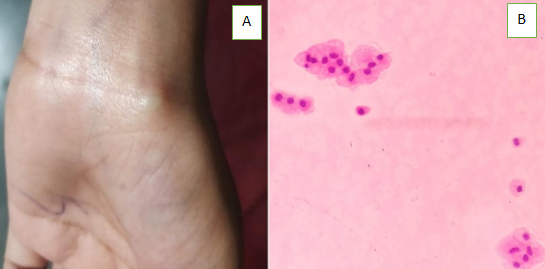
Figure 2
(A) FNA smears from Calcinosis cutis showing crystalloid pinkish granular background. (H&E,10x); (B) Histological section showing dermis with areas of calcification and fibrosis. (H&E, 40x):
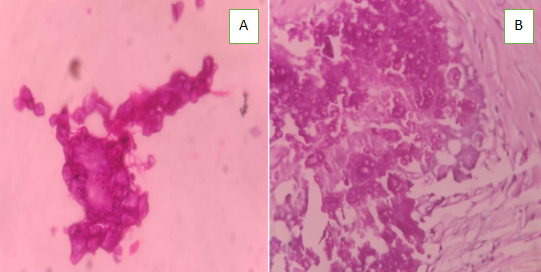
Figure 3
(A) Cytosmear from pilomatrixoma showing clusters of basaloid cells and scattered squamous cells in a background of amorphous material. (Giemsa, 40x); (B) Histological section of pilomatricoma showing shadow cells and basaloid cells. (H&E, 40x).
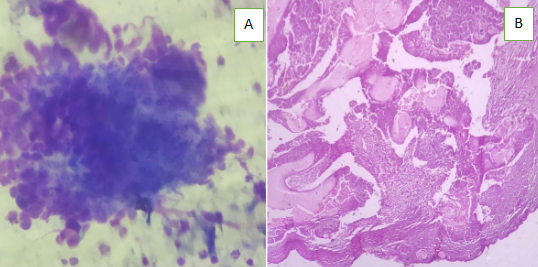
Figure 4
(A) FNA Smear from granular cell tumor showing small clusters and singly scattered large polygonal cells with eccentric nucleus and abundant granular cytoplasm. Background showed some granules and stripped nuclei. (Giemsa, 40x); (B) Histological section from granular cell tumor showing tumor cells arranged in clusters and ribbons separated by dense fibrocollagenous tissue.(H&E, 40x)
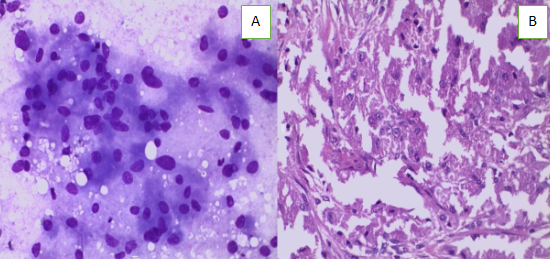
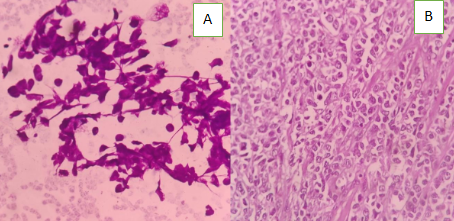
Figure 5
(A) Smear from malignant melanoma showing diffuse population of pleomorphic cells having eccentrically placed hyperchromatic pleomorphic nuclei with intranuclear inclusions, prominent nucleoli and abundant dense cytoplasm with intracytoplasmic pigment. (Giemsa; 40x); (B) Histological section from malignant melanoma showing diffuse infiltration by anaplastic melanocytes in the dermis. (H&E, 40x).
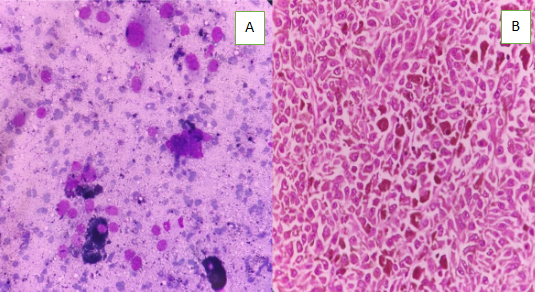
Figure 6
(A) Cytosmears from rhabdomyosarcoma showing loose clusters of small and large pleomorphic cells with high N :C ratio with eccentric placed nuclei and dense cytoplasm. (H&E; 40x) ; ( B) Histological section from embryonal rhabdomyosarcoma showing nests of small round cells with hyperchromatic nuclei and surrounded by fibrous trabeculae. (H&E, 40x ).
Discussion
Role of Fine needle aspiration cytology (FNAC) in the diagnosis of various inflammatory, non-neoplastic and neoplastic lesions of skin, adnexa and soft tissues is well established. Cytology can be used for initial diagnosis of skin lesions, primary benign and malignant soft tissue masses, confirmation of metastatic tumors and for the documentation of local recurrence. However, the exact categorization of the cutaneous and subcutaneous lesions by FNAC, specially of soft tissue tumors is very difficult. It can be attributed primarily due to the heterogeneous nature of the soft tissue tumors as well as absence of tissue architecture in FNAC smears.4 To achieve high diagnostic accuracy in these tumors a thorough familiarity with the histological diversities of soft tissue tumors and experience in cytological interpretation of different cell types is required.5
Skin is a common site to be involved in neoplastic and non neoplastic conditions and occasionally inflammatory lesions can also present as mass lesion. In such cases FNAC of these lesions helps in early timely diagnosis and further appropriate management. Soft tissue is a non epithelial extra skeletal tissue of the body exclusive of reticulo endothelial system, glia, and supporting tissue of the various parenchymal organs. It is represented by the voluntary muscles, adipose tissue, and fibrous tissue along with the vessels serving these tissues. Soft tissue tumors are classified according to the tissue they recapitulate.
The sensitivity, specificity and positive predictive value of FNAC in the diagnosis of soft-tissue tumours is 91.5%, 92.5% and 95.5%, respectively.6 A basic cytological approach towards making a skin and soft tissue tumors diagnosis begins with the familiarity with normal structures, along with identifying myxoid or metachromatic stromal fragments and a variety of dyscohesive cells like spindly, round, pleomorphic, polygonal that are in dicators of a mesenchymal origin on aspirates. These cytological findings are correlated with clinico- radiological findings.7 Advancement in localization of the cutaneous and subcutis with radiological techniques have revolutionized the amount of aspirate one can achieve, especially in deep-seated lesions.8 In the present study, M:F ratio of 1.4:1 was seen which was same as in the study done by Beg et al.9 Similar observation was made by Qui et al, who reported M:F ratio of 1.5:1.10 Maximum number of cases were from the age group of third decade (36.6%) followed by fourth decade (21.7%) which is similar to that observed by Miyaji et al.11 This could be due to non-neoplastic lesions forming major chunk of study group.
In the present study, the lesions were grouped under two main categories: non-neoplastic (38.4%) and neoplastic (61.6%). Among the neoplastic lesions, the benign lesions comprised 96% and malignant ones 4%. In a study of soft tissue lesions of head and neck by Makino et al12 benign neoplasms were 96% and malignant were 4%. Petersen et al13 had done a similar retrospective study and found 49% malignant, 11.4% intermediate, 35% benign, and 4.6% as tumors of uncertain potential. In contrast to our study Kransdorf et al14 reported higher number of malignant soft tissue neoplasms (39.8%) in their study as compared to benign neoplasms (61.2%). Overall in all these studies, benign neoplasms predominated the malignant ones.
In the present study, 27.7% of cases were seen in Upper extremities and axilla followed by head and neck region (22.5%). Lazim et al15 and Zhi-wei et al16 stated that the commonest site for malignant soft tissue lesions was the extremities followed by trunk and abdomen, whereas in a study done by Mandong et al, extremities were the most common site followed by head and neck region.17
In our study, we observed maximum number of cases of Epidermal Inclusion cyst in the non- neoplastic category (45.4%) which correlated well with the histopathological examination. However, one case reported as epidermal cyst on cytology turned out to be pilomatrixoma on histopathology. This could be due to the presence of numerous squamous cells in a dirty background and missing small aggregate of degenerated basaloid cells on cytological smears.
In the present study we also encountered few rare cases comprising of two cases of Calcinosis cutis (0.5%), one case each of Herpes Zoster (0.2%), Molluscum contagiosum (0.2%) and Scar endometriosis (0.2%). Lipoma was the commonest benign neoplastic lesion, comprising 80.5% of all benign tumors. Majority presented as multiple swellings mostly on extremities. Histopathological diagnosis was obtained in 285 out of 552 cases of lipomas; 274 cases showed good correlation. Walaas et al also observed excellent correlation between the two diagnostic modalities for lipomas.18 Eleven discordant cases comprised of five cases of accessory breast tissue, three cases of benign mesenchymal tumor and three cases of tubercular lesion. Rare neoplastic benign cases which were encountered cytologically were single case of lingual schwannoma, subcutaneous granular cell tumor, two cases of infantile Fibromatosis colli. One interesting case of chondroma of scalp was seen histopathologically in a 65 year old male patient which w as misdiagnosed on cytology as a vascular lesion.
Squamous cell carcinoma (51.6%) was the commonest malignant tumor observed in our study. Its prevalence was higher than that observed by Ramzy et al (37%).19 Maximum occurrence was in the head and neck region. Ormsby et al had documented squamous cell carcinoma to occur more commonly on the exposed surface.20 Few interesting and unusual cases were encountered in malignant category too. One case of plasmacytoma was seen which presented as neck swelling in a 45 year old male. However, patient did not undergo histopathological examination. A case of forehead swelling in 52 year old male revealed Malignant adnexal tumor which on histology was confirmed as Sebaceous Carcinoma. One case reported as intermediate grade mesenchymal lesion of foot on cytomorphology turned out to be clear cell sarcoma of soft tissue on histopathological examination.
Conclusion
Although cutaneous and subcutaneous lesions are accessible and easily amenable to surgical excision, FNAC of these lesions is of great help in early timely diagnosis of unusual skin, adnexal and soft tissue masses specially for differentiating reactive/benign process from malignant condition. It is also possible to avoid diagnostic errors in these cases due to overlapping cytological features by paying attention to the possible pitfalls.
