- Visibility 183 Views
- Downloads 146 Downloads
- DOI 10.18231/j.jdpo.2019.055
-
CrossMark
- Citation
Platelet DistributionWidth (PDW): A novel platelet marker in thrombocytosis: An insight
- Author Details:
-
R Shubha Sangeetha *
-
Y A Manjunatha
Introduction
Automated Haematology Analysers measure several haematological parameters automatically along with platelets indices, which are probably the most ignored by clinical lab due to difficulty in standardization, as well as being affected by range of methodological problem. PDW has been receiving attention among all platelet indices due to its usefulness for distinguishing between reactive thrombocytosis and thrombocytosis associated with MPD.[1]
Determination of PDW reference range is fundamental. The association of this parameter with the platelet number and MPV may be used for the diagnosis and differentiation of several pathologies.[1]
Cases with reactive thrombocytosis had low MPV and PDW. Patients with low MPV and PDW and high platelet counts wrongly suggests reactive etiology.[2]
PDW expresses the distribution of the size of platelets produced by the megakaryocytes.[3]
Although platelet parameters such as MPV and PDW have been available now for quite a time, their clinical usefulness hitherto was not obvious, especially as they may be influenced by the delay between blood collection and analysis.[4]
Materials and Methods
This prospective observational study was performed in the Department of Pathology and Central Laboratory of Dr B R Ambedkar Medical College/Hospital. A total of 500 cases were studied out of which 250 were individuals with normal platelet count and 250 cases of patients with platelet count more than 5 lakhs identified during routine CBC ,were included as thrombocytosis cases. PDW values recorded by 7 part auto hematoanalyser using the principle Impendence resistance was tabulated in thrombocytosis patients and PDW values were compared with individuals with normal platelet count and variations in the two groups were analysed. Clinical history and details of other lab parameters in thrombocytosis patients were collected to analyse the possible underlying aetiology. Variations in PDW values were analysed in thrombocytosis patients.
Results
In A total of 500 case study 250 were normal individuals. Age range of the 250 thrombocytosis cases considered for the study was 18years-80years with median age being 49 years.
Out of 250 patients of thrombocytosis 158(63.2%) patients were males and 92(36.8%) patients were females. Male predisposition was observed in Thrombocytosis.([Figure 1] )

Range of thrombocytosis studied was 5.1 to 8.5 lakhs/mm3 with increased median platelet count being 6.8lakhs/mm3
Normal PDW (fl) [Mean+_2SD] determined in our lab was 12.4+_1.8. PDW values in 250 normal individuals were in the above determined normal range.
PDW [Mean+_2SD] determined in 250 cases of thrombocytosis was 16.82+_1.9 with PDW range of 10.28-23.36.
Increase in mean PDW values were seen in patients with thrombocytosis compared to normal individuals.
PDW values more than >14 was observed in 35.2% of cases of Reactive Thrombocytosis cases in our study.
Most common underlying aetiologies for reactive thrombocytosis detected in our study is as follows:
| Etiology | Number of cases |
| 1.Recovery from thrombocytopenia following Cobalamin deficiency treatment (Figure 3 ) and post viral fever (Figure 4 ) | 87(34.8%) |
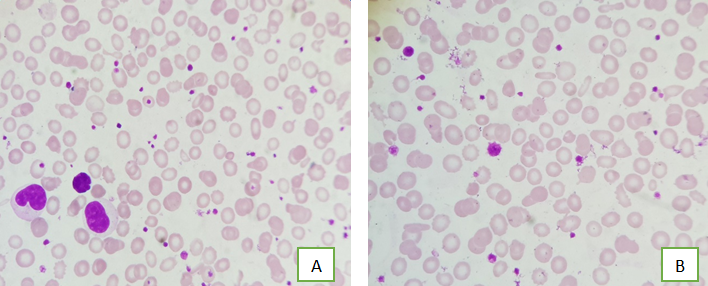
| 2. Iron deficiency anaemia (Figure 1 A&B) | 56 (22.4%) |
| 3. Post surgery | 41(16.4%) |
| 4. C hronic inflammatory disorders | 38(15.2%) |
| 5. Acute Haemorrhage | 17(6.8%) |
| 6..Malignancy (Figure 5 ) | 7(2.8%) |
| 7.Transient thrombocytosis following child birth | 4 (1.6%) |




Discussion
Platelet participates in the pro inflammatory process by releasing proteins and small molecules from their granules which can influence the function of vascular wall and circulating immune cells.[5]
Activation of platelets causes morphological changes, including shape changing from discoid to spherical with pseudopodia formation. Progressively activated platelets can have heterogeneous sizes, performing larger PDW values.[6]
IN addition, PDW can be affected by morphological changes of platelets when the platelet is activated during inflammation and thrombotic processes.[7]
The presence of large platelets has been reported in patients with myeloproliferative disorders on peripheral blood smears. The quantitation of such platelets, however remains subjective.[8]
In our study significant variations in platelet sizes was observed in thrombocytosis cases more commonly associated with IDA(Iron deficiency Anaemia)([Figure 2] B). Large platelets and giant platelets ([Figure 5]) were also identified in certain chronic inflammatory disorders.
Several authors tried to discriminate thrombocytosis in myeloproliferative disorders from reactive thrombocytosis by using platelet parameters provided by blood analysers.[9] Previous studies reveal a correlation between platelet, MPV and PDW suggesting a combined interpretation through calculation of a PDW residual. In 3/4th cases of MPD the PDW residual on its own way is highly suggestive of autonomous thrombocytosis.[10]
The increased PDW residual probably reflects a dysregulation in thrombopoiesis which is also translated by the multiple abnormalities of platelet reactivity and the change in platelet membrane and adenine nucleotide content that have been previously described[8],[11],[12]
PDW is an indicator of volume variability in platelet size and is increased in the presence of platelet anisocytosis.[13]
PDW is the distribution curve with a total curve height of 100%.[14]
PDW directly measures variability in platelet size and changes with platelet activation and reflects the heterogeneity in the platelet morphology.[15]
Under physiological conditions there is direct relationship between MPV and PDW ,both change usually in the same direction.[16] Meanwhile, there are conflicting reports in the literature about the relationship between platelet volumes and number which suggest they are affected.
R.Sridhar Reddy et al;[17] who studied PDW in Thrombocytopenia cases revealed PDW( fl)[mean +_SD] 12.12+_1.99 in control group, the same correlated well with our study with Normal PDW (fl)[Mean+_2SD] determined in our lab was 12.4+_1.8. PDW values in 250 normal individuals were in the above determined normal range.
Amin et al;[18] found that PDW increases in vaso occlusive crisis in sickle cell disease. They concluded that megakaryocytic hyperplasia was responsible for PDW increase.
E Sehayak et al; stated that PDW> or =10.5 was found in 50%, and 21%, of ET, and RT(reactive thrombocytosis)groups respectively which correlated with PDW values in RT cases in our study.
Conclusion
Platelet Indices are simple efficient and economical biomarkers of platelet activation. PDW variations reflects the role of platelets as an inflammatory mediator and directs clinical work up to assess the diagnostic and prognostic values without incurring additional costs in thrombocytosis and hence a novel marker indeed.
Source of Funding
None.
Conflict of Interest
None.
References
- M G Farias, E G Schunk. Dal Bos DeCastro SM definition of reference ranges for the platelet distribution width(PDW): a local need. Clin Chem Lab Med 2010. [Google Scholar]
- N N Syed, N Usman, M Khurshid. Thrombocytosis: age dependent aetiology and analysis of Platelet indices for Differential Diagnosis Indian. J Pathol Microbiol 2007. [Google Scholar]
- Claude Osselaer, Jacques Jamant. Jean Marie Scheiff- PDW for differentioal diagnosis of Thrombocytosis. Clin Chem 1997. [Google Scholar]
- S R Jackson, J M Carter. Platelet: lab measurement of clinical application. Blood Rev 1993. [Google Scholar]
- E Schayek, N Ben-Yosef, M Modan, A Chetrit. platelet parameters and aggregation in essential and reactive Thrombocytosis. Am J Clin Pathology 1998. [Google Scholar]
- B M Small, R E Bettigole. Diagnosis of MPD by analysis of platelet volume distribution. Am J Clin Pathology 1981. [Google Scholar]
- G Leoncini, M Maresca, E Buzzi, A Piana, U Armani. Platelets of patients affected with ET are abnormal in plasma membrane and adenine nucleotide content. Europe J Haematol 1990. [Google Scholar]
- P Kaywin, M Mc Donough, P A Insel, P J Shattil. Platelet function in ET. N Engl J Med 1978. [Google Scholar]
- Y U Budak, M Polat, K Huysal. The use of platelet indices, platelet crit, MPV and PDW in emergency non- traumatic abdominal surgery : a systematic review. Biochem Med 2016. [Google Scholar]
- G Lippi, F Pavesi, Pipitones .. Evaluation of MPV with four haematological analyzers: harmonization is still an unresolved issue. Blood Coagulation Fibrinolysis 2015. [Google Scholar]
- Van der Lelie J, Von dem Borne AK. Platelet volume analysis for differential diagnosis of Thrombocytosis. J Clin Pathology 1986. [Google Scholar]
- B Dinc, - Oskay, B S E Dinc, - Bas, - Tekin. New parameter in diagnosing acute appendicitis : Platelet Distribution Width. World J Gastroenterol 2015. [Google Scholar]
- V Wiwanitkit. Platelet crit, mean platelet volume, platelet distribution width: its expected values and correlation with parallel Red Blood Cell parameters. Clin Appl Thrombosis/ Hemostasis 2004. [Google Scholar]
- Iii Al Frelinger, A S Torres, A Caiafa. Platelet rich plasma stimulated by pulse electric fields: platelet activation, pro-coagulant markers, growth factor release and cell proliferation. Platelets 2015. [Google Scholar]
- A T Sayit, P H Gunbey, Y Terzi. Is the mean platelet volume in patients with acute cholecystitis an inflammatory marker?. J Clin Diagn Res 2015. [Google Scholar]
- E E Vagdatli, I Gouriari, - Labrianou. Platelet Distribution Width: A simple practical marker of activation of coagulation. Hippokratia 2010. [Google Scholar]
- Y Park, N Schoene, W Harris. MPV as an indicator of Platelet activation Methodological issues. Platelet 2002. [Google Scholar]
- M A Amin, A P Amin, H R Kulkarni. PDW is increased in vaso occlusive crisis in sickle cell disease. Ann Haematol 2004. [Google Scholar]
