- Visibility 112 Views
- Downloads 19 Downloads
- DOI 10.18231/2581-3706.2019.0013
-
CrossMark
- Citation
Spectrum of skin lesions including skin adnexal tumors in a North Indian tertiary care hospital
- Author Details:
-
Megha Bansal
-
Nikhilesh Kumar
-
Monika Gupta
-
Honey Bhasker Sharma *
Abstract
Aims: This study was undertaken in a tertiary care hospital in North Indian state of Uttar Pradesh to evaluate the pattern of skin diseases and various skin neoplasms in biopsy specimens.
Material and Methods: A retrospective analysis of 109 skin biopsies was undertaken. The neoplasms were categorised as per International Classification of World Health Organization.
Results: Keratinous cyst (59 cases) was the most common non- neoplastic skin lesion and it represented 79.7% of non- neoplastic skin lesions. The most common neoplastic skin lesions were soft tissue tumors of vascular origin encompassing pyogenic granuloma which was 34.2% of skin tumors. Commonest malignant neoplasm was squamous cell carcinoma which is categorized under classification of keratinocytic tumors of skin.
Conclusion: Histopathological examination is essential for the diagnosis and classification of various skin lesions including skin tumors which helps in proper treatment of the patient.
Keywords: Dermatological, Keratinocytic, Follicular.
Introduction
Dermatological disorders are very common. They may be intrinsic to the skin or may arise as manifestations of systemic disease.[1] Despite the advances in molecular techniques, diagnosis and prognosis, morphology is still the basis of diagnosis for most neoplasms and many inflammatory skin lesions.[2] It is necessary that clinical differential diagnosis be correlated with gross and microscopic observations in order to render a clinically relevant diagnosis.[3] The pattern of skin diseases varies from country to country and various geographical regions of the same country.[4]
Skin tumors encompass a wide variety of benign and malignant neoplasms of skin and subcutis that are classified and differentiated as keratinocytic, melanocytic, appendageal, haemato-lymphoid and soft tissue tumors.[5]
This study was based on evaluating all the non-neoplastic skin lesions as well as benign and malignant tumors of skin and sub-cutis based on histopathological diagnosis.
Aims and objectives
To retrospectively study the histopathological spectrum of skin lesions with special reference to skin tumors as prevalent in North Indian state of Uttar Pradesh.
Materials and Methods
This is a two and a half-year retrospective study of 109 cases of skin biopsies received in the Department of Pathology in a tertiary care teaching hospital- T. S. Misra Medical College and Hospital, Lucknow, Uttar Pradesh and was undertaken from December 2015 to May 2018. Patients history, age, site of lesion and character were noted. The slides were taken out from filing and reviewed.
Results
A total of 109 cases were evaluated. The age distribution pattern revealed that the maximum skin lesions (non-neoplastic) were in the age range of 21 to 30 years (24%) and 31 to 40 years (24%) and skin tumors in 41 to 50 years age group (23.5%). – Table 1
Table 1: Age Group.
|
Age range |
No. of skin lesions |
% of skin lesions |
No. of skin tumors |
% of skin tumors |
|
0-10 |
02 |
2.6 |
01 |
2.9 |
|
11-20 |
15 |
20 |
05 |
14.7 |
|
21-30 |
18 |
24 |
04 |
11.7 |
|
31-40 |
18 |
24 |
04 |
11.7 |
|
41-50 |
11 |
14.6 |
08 |
23.5 |
|
51-60 |
04 |
5.3 |
06 |
17.6 |
|
61-70 |
07 |
9.3 |
03 |
8.8 |
|
71-80 |
00 |
0 |
02 |
5.8 |
|
>80 |
00 |
0 |
01 |
2.9 |
The incidence of dermatological disease was more in males (62.3%) than females with a male to female ratio of 1.65.
The anatomic distribution pattern showed that the maximum number of cases (both skin lesions and tumors) involved head and neck region (68.8%) followed by extremities (14.6%)-Table 2.
Table 2: Location.
|
Location |
Skin lesions |
Skin tumors |
|
Extremity |
06 |
10 |
|
Head and neck |
58 |
17 |
|
Shoulder and back |
04 |
04 |
|
Trunk and abdomen |
05 |
01 |
|
Others |
01 |
03 |
Out of a total of 109 skin lesions, 74 lesions were non-neoplastic (67.9%) and there were 35 skin tumors (32.1%).
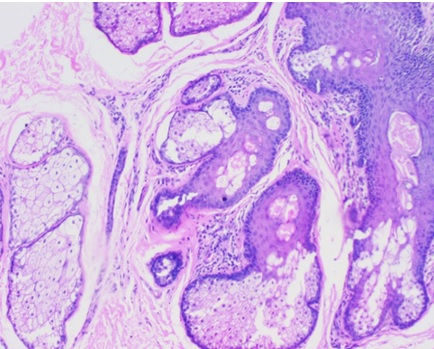
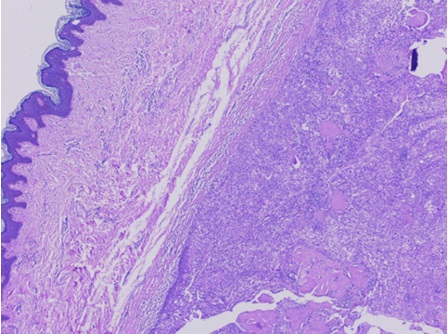
The most common non- neoplastic skin lesion was keratinous cyst (59 cases) which was 79.7% of non- neoplastic skin lesions. Granulomatous lesions, nevus sebaceous, dermoid cyst, trichilemmal cyst, calcinosis cutis, rhinoscleroma and hamartoma were among the other non-neoplastic lesions encountered-Table3. The nevus sebaceous diagnosed shows basaloid proliferations along with prominent and increased sebaceous lobules. [Fig. 1].The most common benign neoplastic skin lesions were soft tissue tumors encompassing pyogenic granuloma which constituted 34.2% of skin tumors followed by keloid which were 11.4% of skin tumors- Table4.
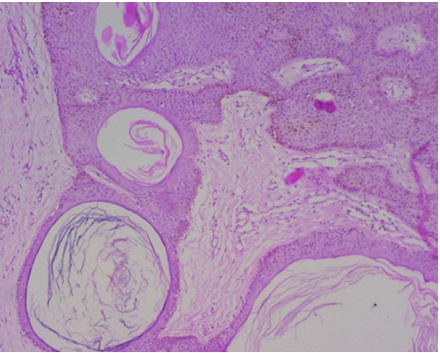
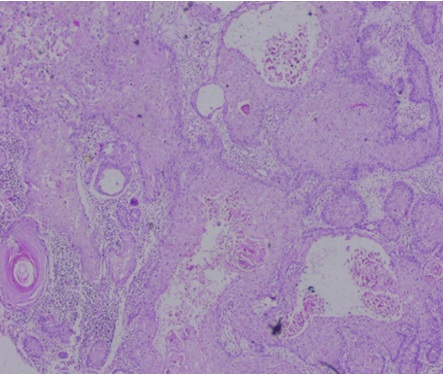
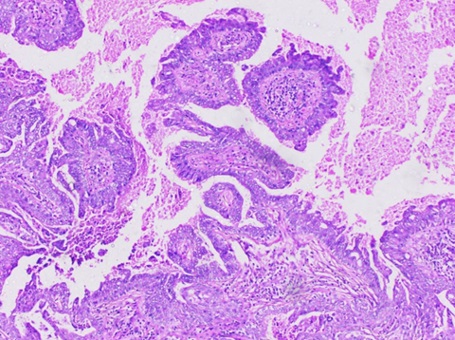
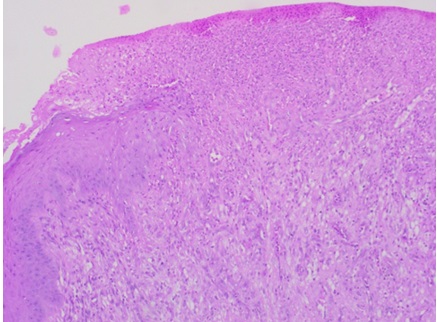
The most common malignant skin tumor found in our study was squamous cell carcinoma- keratinocytic tumor (11.4% of skin tumors). Other keratinocytic tumors included verruca vulgaris, seborrhoeic keratosis and basal cell carcinoma-Table 4. Seborrhoeic keratosis in our study on microscopic examination showed acanthotic basaloid cells along with characteristic pseudo-horn cysts [Fig. 2]. The squamous cell carcinoma shows nests and tongues of malignant squamous cells showing significant cytologic atypia. A keratin pearl is also noted [Fig. 3].
The appendageal tumors revealed tumors of follicular differentiation like trichilemmoma-2.8%, trichoepithelioma-8.5%, tumors of apocrine differentiation like syringocystadenoma papilliferum-2.8% and tumors of eccrine differentiation- eccrine acrospiroma-2.8%.
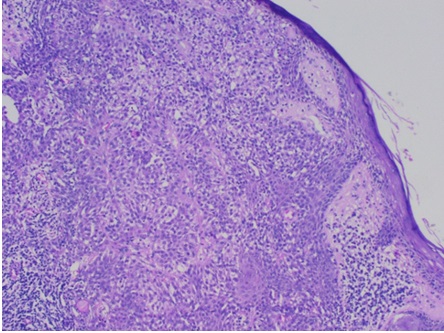
Sections from trichilemmoma shows downwards growth of epithelial cells which show clear cell differentiation [Fig. 4]. Eccrine acrospiroma shows a lining of stratified squamous epithelium with underlying dermis displaying sheets of tumor cells with pale eosinophilic cytoplasm along with some cystic spaces [Fig. 5]. Histopathology of syringocystadenoma papilliferum shows glandular papillary fronds lined by cuboidal to columnar cells, projecting into the cystic lumen [Fig. 6]. Pyogenic granuloma on microscopic sections show vascular proliferation along with inflammation with overlying thinned out epidermis showing ulceration and acanthosis seen at the sides [Fig. 7].
Table3: Distribution of skin lesions (non-neoplastic):
|
Skin lesion |
Number of cases |
Percentage of cases (among non-neoplastic) |
Overall percentage |
|
Keratinous cysts |
59 |
79.7 |
54.1 |
|
Trichilemmal cyst |
02 |
2.7 |
1.8 |
|
Dermoid cyst |
03 |
4.0 |
2.7 |
|
Nevus sebaceous |
03 |
4.0 |
2.7 |
|
Calcinosis cutis |
02 |
2.7 |
1.8 |
|
Rhinoscleroma |
01 |
1.3 |
0.9 |
|
Granulomatous lesions |
03 |
4.0 |
2.7 |
|
Hamartoma |
01 |
1.3 |
0.9 |
Table 4: Distribution of skin tumors (neoplastic):
Keratinocytic tumors
|
Skin tumor |
Number of cases |
Percentage of cases (among neoplastic) |
Overall percentage |
|
Verruca |
|
|
|
|
Verruca vulgaris |
02 |
5.7 |
1.8 |
|
Acanthomas |
|
|
|
|
Seborrheic keratosis |
03 |
8.5 |
2.7 |
|
Basal cell carcinoma |
02 |
5.7 |
1.8 |
|
Squamous cell carcinoma |
04 |
11.4 |
3.6 |
|
Others |
|
|
|
|
Clear cell tumor (metastasis) |
01 |
2.8 |
0.9 |
Appendageal tumors:
|
Skin tumor |
Number of cases |
Percentage of cases ( among neoplastic) |
Overall percentage |
|
Follicular differentiation |
|
|
|
|
Trichilemmoma |
01 |
2.8 |
0.9 |
|
Trichoepithelioma |
02 |
5.7 |
1.8 |
|
Desmoplastic trichoepithelioma |
01 |
2.8 |
0.9 |
|
Apocrine differentiation |
|
|
|
|
Syringocystadenoma Papilliferum |
01 |
2.8 |
0.9 |
|
Eccrine differentiation |
|
|
|
|
Eccrine acrospiroma |
01 |
2.8 |
0.9 |
Soft tissue tumors:
|
Skin tumor |
Number of cases |
Percentage of cases ( among neoplastic) |
Overall percentage |
|
Vascular tumors |
|
|
|
|
Pyogenic granuloma |
12 |
34.2 |
11.0 |
|
Fibrous, fibrohistiocytic and histiocytic tumors |
|
|
|
|
Keloid |
04 |
11.4 |
3.6 |
|
Dermatofibroma |
01 |
2.8 |
0.9 |
Discussion
In the present retrospective study, the maximum number of biopsies were in the age group of 31-40 years. Of these the non-neoplastic skin lesions were common in the 21-40 years age group and skin tumors in the 41-50 yrs. This was in contrast to reports by Thamiselvi et al and Sunita et al who recorded the most common age group of >50 years.[1],[6]
All the skin lesions including tumors were more common in males (62.3%). This was comparable to studies by Rakesh et al - males 56% and Thamiselvi et al - males 64.6%.[7],[6]
Majority of skin lesions were seen in the head and neck region-68.8% followed by extremities in our study. Ankit et al also reported most tumors in head and neck region.[8] Thamiselvi reported maximum lesions in extremities -36.5% followed by head and neck region.[6]
Out of 109 skin biopsies received, 74 lesions were non-neoplastic i.e 67.9% and there were 35 skin tumors.
Keratinous cyst was the most common lesion recorded-79.7% of non-neoplastic lesions in our study. This was comparable to study by Ha and Kim.[9] Other non-neoplastic lesions diagnosed were granulomatous lesions, dermoid cyst, nevus sebaceous, trichilemmal cyst, calcinosis cutis, rhinoscleroma and hamartoma.
The skin tumors in this study were classified into keratinocytic tumors, appendageal tumors and soft tissue tumors.
The most common keratinocytic tumors were squamous cell carcinoma (11.4% of tumors), followed by seborrhoeic keratosis (8.5%), verruca vulgaris (5.7%) and basal cell carcinoma (5.7%).
One case with secondaries in skin reported as clear cell tumor was also included.
Squamous cell carcinoma was reported as the most common malignancy followed by Basal cell carcinoma by Sheenam et al and Gundalli et al which was comparable to our study.[10],[11] This was in contrast to study by Khalid who reported Basal cell carcinoma as the most common tumor followed by Squamous cell carcinoma.[12]
Among the appendageal tumors, our study comprised tumors of follicular differentiation, apocrine differentiation and eccrine differentiation. The most common appendageal tumor recorded was Trichoepithelioma (8.5%), of which one case reported was of desmoplastic variant. This was comparable to study by S Gayatri et al who also reported Trichoepithelioma as the commonest adnexal tumor.[13]
Ankit et al reported most adnexal tumors in the head and neck region which was similar to our study.[8]We had two cases of trichoepithelioma in the scalp and third case in infra-orbital region of face. Our study was also comparable to study by Radhika et al in which two cases of trichoepithelioma were reported in scalp.[14] Study by Abanti Sinha et al showed that all cases of Trichoepithelioma were distributed around nose.[15]
Other adnexal tumors reported in our study were Trichilemmoma, Syringocystadenoma papilliferum and Eccrine acrospiroma.
The adnexal tumors in our study were found in young age group of 11-20 years, which was comparable to study by Nair et al.[16]
The most common soft tissue tumor found in our study was pyogenic granuloma-34.2% which was also the most common skin tumor found in our study. The second most common soft tissue tumor found was keloid. One case of Dermatofibroma was also included among fibrohistiocytic cutaneous soft tissue tumors.
 |
Click here to view |
Fig. 1: Nevus Sebaceous
 |
Click here to view |
Fig. 2: Seborrhoeic keratosis
 |
Click here to view |
Fig. 3: Squamous cell carcinoma
 |
Click here to view |
Fig. 4: Trichilemmoma
 |
Click here to view |
Fig. 5: Eccrine Acrospiroma
 |
Click here to view |
Fig. 6: Syringocystadenoma papilliferum
 |
Click here to view |
Fig. 7: Pyogenic granuloma
Conclusion
As per our study, in our area which is in the northern part of India, cystic lesions (keratinous cysts) were the commonest skin lesions, followed by vascular soft tissue tumors (cutaneous pyogenic granuloma).
Conflict of Interest: None.
References
- a, b Singh S, Debnath A, Datta D, Chakravarty S, Chaubey RN. Histopathological evaluation of skin lesions with special reference to Skin Adnexal tumours in a tertiary care centre of North-Eastern India- A three-year study. IOSR-J Dent Med Sci 2016;15(2):34-39.
- ^ Elder DE (ed.). Lever’s histopathology of the skin. 10th ed. Philadelphia: Lippincott Williams and Wilkins. 2008
- ^ Rosai J. Rosai and Ackermanns Surgical Pathology. 10th ed. Edinburgh: Mosby. Chapter 4 - Skin
- ^ Rook A, Savin JA, Wilkinson DS. The prevalence, incidence and ecology of diseases of skin: Textbook of dermatology. Oxford: Oxford University Press. 1987:39-53
- ^ Le Boit PE, Burg G, Weedon D, Sarasain A. World Health Organisation Classification of Tumors. Pathology and genetics of skin tumors. Lyon: IARC Press: 2006.
- a, b, c Thamiselvi R, Sivakami K, Pammysinha, Subramaniam PM. Clinico-morphological study of skin diseases. Int J Res Rev 2014; 6(14):54-57.
- ^ Mehar R, Ravi J, Kulkarni CV, Narang S, Mittal M. Histopathological study of Dermatological lesions- A Retrospective Approach. Int J Med Sci and Public Health 2014;3(9).
- a, b Sharma A, Paricharak D, Nigam JS, Rewri S, Bhatia P. Histopathological study of skin Adnexal Tumors- Institutional Study in South India. J Skin Cancer 2014.
- ^ Ha SJ, Kim SY. A study on skin tumors in the Suwon and South Kyunggido Area. Korean J Dermatol 1996; 34(2):199-205.
- ^ Azad S, Acharya S, Kudesia S, Kishore S, Mehta A. Spectrum of skin tumors in a tertiary care centre in Northern India. J Evol Med Dent Sci 2014;3(64).
- ^ Gundall S, Kolekar R, Pai K, Kolekar A. Histopathological Study of Skin Tumors. Int J Healthcare Sci 2014- 2015; 2(2):155-163.
- ^ Aboud K, Hawsawi K, Bhat M, Ramesh V, Ali S: Skin cancers in Western Saudi Arabia. Saudi Med J 2003;24(12):1381-1387.
- ^ Gayathri S, Alavandar E, Kumar A: An analysis of skin appendageal tumors in South India. J Evol Med Dent Sci 2012;1(6).
- ^ Radhika K, Phaneendra BV, Rukmangadha N, Reddy MK. A Study of biopsy confirmed skin adnexal tumors: experience at a tertiary care teaching hospital. J Clin Sci Res 2013;2:132-138
- ^ Saha A, Das NK, Gharami RC, Chowdhury SN, Datta PK. A Clinico-pathological study of appendageal skin tumors, affecting head and neck region in patients attending the dermatology OPD of a tertiary care centre in Eastern India. Indian J Dermatol 2011;56(1):33-36.
- ^ Nair PS, Sadan K, Mukku T: A Clinicopathologic study of skin appendageal tumors. Indian J Dermatol Venereol Leprol 2008;74(5):550.
How to Cite This Article
Vancouver
Bansal M, Sharma HB, Kumar N, Gupta M. Spectrum of skin lesions including skin adnexal tumors in a North Indian tertiary care hospital [Internet]. IP J Diagn Pathol Oncol. 2025 [cited 2025 Sep 05];4(1):67-71. Available from: https://doi.org/10.18231/2581-3706.2019.0013
APA
Bansal, M., Sharma, H. B., Kumar, N., Gupta, M. (2025). Spectrum of skin lesions including skin adnexal tumors in a North Indian tertiary care hospital. IP J Diagn Pathol Oncol, 4(1), 67-71. https://doi.org/10.18231/2581-3706.2019.0013
MLA
Bansal, Megha, Sharma, Honey Bhasker, Kumar, Nikhilesh, Gupta, Monika. "Spectrum of skin lesions including skin adnexal tumors in a North Indian tertiary care hospital." IP J Diagn Pathol Oncol, vol. 4, no. 1, 2025, pp. 67-71. https://doi.org/10.18231/2581-3706.2019.0013
Chicago
Bansal, M., Sharma, H. B., Kumar, N., Gupta, M.. "Spectrum of skin lesions including skin adnexal tumors in a North Indian tertiary care hospital." IP J Diagn Pathol Oncol 4, no. 1 (2025): 67-71. https://doi.org/10.18231/2581-3706.2019.0013
