Author Details :
Volume : 4, Issue : 1, Year : 2019
Article Page : 63-66
https://doi.org/10.18231/2581-3706.2019.0012
Abstract
Introduction: Extrapulmonary tuberculosis in form of lymphonodes is the common presentation of tuberculosis in developing countries. Fine needle aspiration cytology helps in early diagnosis & treatment for tubercular lymphadenitis, which remains the cornerstone for the effective management of the disease.
Aim: To study the cytological characteristics and compare with the bacteriological load with the help of Zeihl Neelsen stain.
Materials and Methods: 445 smears were studied for a period of one year. Smears were categorized into 4 patterns Pattern A - epithelioid cell granulomas without caseous necrosis, Pattern B -epithelioid cell granulomas with caseous necrosis, Pattern C- caseous necrosis without granuloma, Pattern D – neutrophils with abundant caseous necrosis. Bacillary load was graded as 1+, 2+ and 3+ were compared with the cytological categories. A p value of <0>
Results: Pattern A was observed in 16.7% cases, Pattern B in 18.3%, Pattern C in 37.8% & Pattern D in 27.2% of cases. Statistical significance was seen between cytomorphological pattern & AFB grade (p=0.026 & X2=20.0639). It was found that pattern C& D showed the highest AFB grade of 3+ by a 2x2 analysis to test the degree of one hypothesis.
Conclusion: FNAC is an useful tool in the early diagnosis of tubercular lymphadenitis avoiding the un necessary burden of surgical intervention. Maximum bacillary load was correlated with the patterns C & D.
Keywords: Fine needle aspiration cytology, Tuberculosis, Lymph nodes, Caseous necrosis, Acid fast bacilli.
Tuberculosis is a major public health problem worldwide, especially in the developing countries like India. Peripheral lymphadenopathy is the most common manifestation of extrapulmonary tuberculosis.[1],[2]Fine Needle Aspiration Cytology (FNAC) is safe, cost effective and conclusive procedure.[3] It provides an alternative to excision biopsy for lymph nodes and is an easy procedure for collection of material for cytomorphological and bacteriological examination.[4] The aim of this study was to describe various cytomorphological patterns of tuberculous lymphadenitis and to assess correlation between FNAC and Ziehl-Neelsen (ZN) staining in diagnosing tuberculous lymphadenitis.
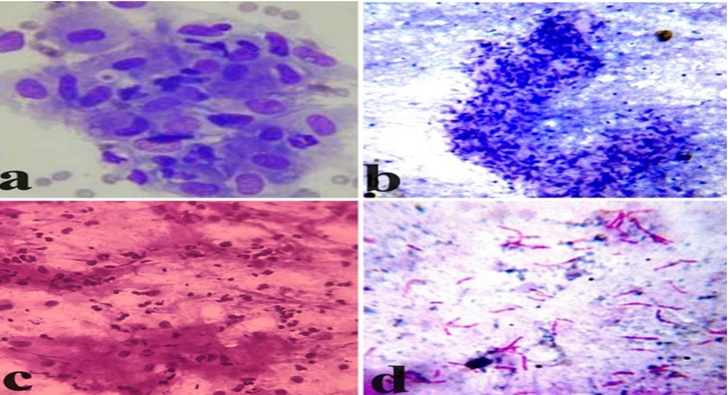
This retrospective study was done for a period of one year in the Department of Pathology April 2017 to March 2018. Five hundred and forty consecutive cytology smears from superficial lymph nodes, archived and cytological proven to have tuberculosis were included in the study. Cytological diagnosis of tuberculosis was rendered to those cases with granulomatous lymphadenitis with or without caseous necrosis and/or cases positive for Tubercle bacilli by ZN stain. In each case, brief clinical history and physical examination findings were recorded from the medical records. Relevant investigations, whenever available, were also recorded. None of the cases included showed evidence of atypical mycobacteria or were HIV positive or immunocompromised. Smears were stained with Hematoxylin & Eosin, Papanicolou and Giemsa stain The smears were grouped into four categories based on the morphological features (Fig 1),[5],[6]
The findings of ZN staining was labeled as positive for acid fast bacilli (AFB), when there is presence of pink beaded and stumpy rod shaped organisms under X1000 (oil immersion) objective. The positive smears were semi quantitatively graded into three grades. The cases which showed occasional bacilli were graded 1+, cases with singly scattered bacilli were graded 2+, while cases which showed numerous bacilli which were singly dispersed or arranged in bundles were graded as 3+.[7],[8]Data was analyzed using SPSS version 15 for Windows (Statistical Package for the Social Sciences, Chicago, IL, USA). A p value of <0>
From the previous records available in the department of Pathology 540 cases which were diagnosed as tubercular lymphadenitis on cytology were included in the study. The age of patients ranged from 2 to 75 years with a median age of 28 years. The distribution of cases among various age groups & sex is given in Table-1. Second and third decades were the most affected. There were 229 males and 311 female patients in the present study making the male to female ratio as 1:1.36. Among the various sites of lymphnode involvement, cervical nodes were the most common (73.1%), followed by axillary and generalized lymphadenopathy. Inguinal group of lymph nodes were the least involved group (Table 2). Grossly 158 cases (29.26%) yielded cheesy caseous material, 110 cases yielded purulent material, while remaining cases yielded blood mixed aspirate 272 (50.38%).
On the basis of cytomorphology tubercular lymphadenitis were categorized into 4 patterns (Table 3). Pattern A was observed in 16.7% cases, Pattern B in 18.3%, Pattern C in 37.8% & Pattern D in 27.2% of cases. The overall AFB positivity was 61.86% (334/540 cases). Statistical correlation between AFB positivity & different cytomorphological pattern was seen (p<0>[2]=212.9813). AFB positivity was highest in pattern C (83.8%), followed by Pattern D (81.6%). Pattern A showed the least AFB positivity (Table 3).
It was noted that the cases which yielded cheesy and purulent material demonstrated pattern C & D, while pattern A & B was observed when blood mixed aspirate was present. Similarly the AFB positivity was highest among cases which yielded cheesy & purulent material (69%), while blood mixed aspirate yielded lowest rate of AFB positivity (26%). Table 4 shows bacillary load among AFB positive cases. 137 cases showed 1+ grade (41%); 113 cases showed 2+ grade (33.83%) and 84 cases showed 3+ AFB grade (25.15%). Statistical significance was seen between cytomorphological pattern & AFB grade (p=0.026 & X2=20.0639). It was found that pattern C& D showed the highest AFB grade of 3+ by a 2x2 analysis to test the degree of one hypothesis.
Table 1: Age and Sex distribution of Tubercular Lymphadenitis
|
Age group (years) |
Males |
Females |
Total |
Percentage |
|
0-10 |
38 |
37 |
75 |
13.9 |
|
11-20 |
55 |
71 |
126 |
23.3 |
|
21-30 |
74 |
93 |
167 |
31 |
|
31-40 |
27 |
42 |
69 |
12.8 |
|
41-50 |
14 |
34 |
48 |
8.9 |
|
51-60 |
11 |
23 |
34 |
6.3 |
|
>60 |
10 |
11 |
21 |
3.9 |
|
Total |
229 |
311 |
540 |
100 |
Table 2: Lymph node groups involved in Tubercular lymphadenitis
|
Site |
No. of Cases |
Percentage |
|
Cervical |
395 |
73.1 |
|
Axillary |
70 |
13 |
|
Inguinal |
26 |
4.8 |
|
Generalized |
49 |
9.1 |
|
Total |
457 |
100 |
Table 3: Cyto-morphological features in tuberculous lymphadenitis correlating with AFB positivity
|
Pattern |
Cyto-morphological features |
No. of cases |
Percentage
|
No. of cases with AFB positivity |
Percentage of AFB positivity |
|
A |
Epithelioid cell granulomas without caseous necrosis |
90 |
16.7 |
4 |
4.4 |
|
B |
Epithelioid cell granulomas with caseous necrosis |
99 |
18.3 |
39 |
39.4 |
|
C |
Caseous necrosis with or without occasional epithelioid cells |
204 |
37.8 |
171 |
83.8 |
|
D |
Necrosis with polymorphs |
147 |
27.2 |
120 |
81.6 |
|
|
Total |
540 |
|
310 |
|
Table 4: Correlation between cytomorphological patterns & AFB grading
|
Pattern |
Grading |
||
|
1+ |
2+ |
3+ |
|
|
A |
3 |
1 |
0 |
|
B |
26 |
10 |
3 |
|
C |
59 |
67 |
45 |
|
D |
47 |
35 |
38 |
|
Total |
137 |
113 |
84 |
 |
Click here to view |
Fig. 1: a. Pattern A showing epithelioid cell granuloma (Giemsa, x400). b. Pattern B showing granuloma with caseous necrosis (Papanicolaou stain x100). c. Pattern D – neutrophils with caseous necrosis (H&E x200),. d. Grade 3+ AFB (ZN Stain x1000)
Accurate and timely diagnosis together with effective treatment is the mainstay of tuberculosis care and control.[9] A confirmed diagnosis of tuberculosis can only be given on isolating the M. tuberculosis or finding specific DNA sequence of the bacteria in aspirates. In the resource-poor countries, however, these tests are not within the reach of every individual. In these countries, cost-effective techniques, such as, sputum smear microscopy and morphological features are the corner stone of tuberculosis diagnosis.[10] Extra pulmonary tuberculosis commonly presents as superficial lymphadenopathy. Fine needle aspiration cytology (FNAC) is a very useful and reliable test in these cases, which provides an early morphological diagnosis.[11]
Prasoon D[12] has opined that the immunological response of tubercle bacilli in extra pulmonary cases is similar to that seen in pulmonary cases. Type IV delayed hypersensitivity reaction, seen after 2-4 weeks of infection leads to secretion of ? interferon and TNF ?. These immunologic mediators activate the macrophages to form granulomas in order to phagocytose & kill the organism. When the immunity of the host is decreased, there is ensuing tissue destruction in the center is represented by caseous necrosis containing large number of bacilli. High degree of hypersensitivity reaction leads to infiltration by neutrophils in the necrotic foci. Hence few bacilli are seen in the setting of only granulomatous reaction, while abundant bacilli are seen in predominantly necrotic reaction with little or no granulomas.[12]The results in our study can be explained by this phathophysiology of the organism.
AGE- Tuberculous lymphadenopathy in our study was seen in all age groups, although the majority of the cases were in the second and third decade. This was also observed
in studies done by Nidhi P et al, Chand P et al & Hemalatha A et al.[5],[6],[13]
SEX- Female preponderance was noted in this study with male to female ratio of 1:1.36, which was also reported by Nidhi P et al & Purohit MR et al.[5],[14]
SITE – Cervical group of lymph nodes were the most affected group (73.1%) and inguinal group being the least involved, which was similar to the data published in the literature.[15]Masilmani S et al have opined that this is due to the easy access of the organism through the tonsillar lymphoid region to the cervical lymphnodes.[16]
PATTERN- Various patterns or categories are used to describe the cytomorphological features of tuberculosis.[4],[5],[6],[12],[13],[17]In the current study Pattern C (37.8%) was the predominant pattern followed by Pattern D(27.2%), which was concordant with studies done by Nidhi P et al.[5]
AFB POSITIVITY- Varying AFB positivity has been described in literature from 35.6% to 55.2%.[4],[6],[13],[17]The overall AFB positivity in our study was 61.86%. Chand P et al have reported 44.54%, while in a study done at a tuberculosis referral center by Nidhi P et al, AFB positivity was reported as 71%.[6],[5]In highly suspicious cases of tuberculosis, additional slides can be re-stained with ZN stain to increase the AFB detection rate.[5]Whenever feasible a repeat FNAC can also be attempted.
When AFB positivity was correlated with the various patterns, the highest detection rate of AFB was seen in Pattern C (83.8%) followed by Pattern D (81.6%), which is similar to the findings of Nidhi P et al.[5]Chand P et al have reported 94.1% AFB positivity in cases displaying caseous necrosis & 52.8% in cases with caseous necrosis along with degenerated inflammatory cells.6 Ergete W et al & Das DK et al have reported 68.7% & 77.4% of AFB positivity in cases having caseous necrosis with/without neutrophils respectively.[4],[17]AFB positivity was the least in cases with only granulomas, in all these series, which was observed in our study also.4,5,6,17
MATERIAL OF ASPIRATION & AFB POSITIVITY –Aspirate which yielded cheesy or purulent material had the highest AFB positivity (69%) in the current study, which was also reported by the other studies.[5],[6],[18]Prasoon D has also opined that AFB finding chance will be the highest in cases yielding cheesy or purulent aspirate.[12] A differential diagnosis of acute suppurative lymphadenitis or caseous lymphadenitis is entertained when purulent material is aspirated. However, clinically the enlarged lymph node does not show signs of acute inflammation in the form of local rise of temperature or redness in a case of tuberculous lymphadenitis. Nonetheless all cases of purulent aspirate warrants a ZN stain to detect AFB. It has to be also noted that in metastatic deposit in lymph nodes, especially in elderly patients, a purulent material can be the aspirated. Hence a thorough search for atypical viable cells has to be made or a repeat aspirate from the periphery of the lymph node has to be performed in these cases.
GRADING- Similar to studies done by Hemalatha A et al & Masilmani S et al, there was statistical significant correlation between cytomorphological pattern & AFB grade.[13],[16]It was also noted that in the combined group of pattern C & D,the possibility of finding AFB was the highest. However >10000 bacterial organisms/ml of the sample are required for AFB detection by ZN stain. Those cases with high suspicion of tuberculosis, but with no AFB on ZN stain, has to be subjected to other methods of detecting the bacilli like culture, or cartridge based nucleic acid amplification tests.[3]
Conclusion
The present study confirms that FNAC of lymphnodes is an excellent first line method, for investigating the nature of the lesions and the immunological response. Also combination of fine needle aspiration cytology with acid fast staining is highly valuable for routine diagnosis of tuberculosis. It gives valuable insight into the disease burden in the patient. Other ancillary investigations can be reserved for cases, in which there is a strong clinical suspicion with equivocal result of FNAC and acid-fast staining. It is an economical and convenient alternative to open biopsy of lymph node. The diagnostic accuracy of FNAC can be further improved manifold when used in conjunction with other special techniques like cytochemistry, bacteriologic culture, immuno-cytochemistry, ultrastructural studies and molecular hybridization.
Conflict of Interest: None.
How to cite : Shilpa G, Prasad C , A cytological study of smear characteristics and its correlation with bacillary load in tubercular lymphadenopathy. IP J Diagn Pathol Oncol 2019;4(1):63-66
This is an Open Access (OA) journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
Viewed: 4107
PDF Downloaded: 482