Author Details :
Volume : 4, Issue : 1, Year : 2019
Article Page : 45-49
https://doi.org/10.18231/2581-3706.2019.0008
Abstract
Introduction: Giant cell tumour (GCT) is a common benign bone tumour. Common sites of occurrence in decreasing order of frequency are distal femur, proximal tibia, distal radius. Less frequent sites include distal humerus, pelvis and sacrum.
Aims and Objectives: The aim was to highlight the increasing incidence of common GCT’s in uncommon sites such as distal humerus
Materials and Methods: We present our series of eight cases (M:F::2:6) of distal humeral GCT between 2008-2017. The diagnosis was confirmed by trucut biopsy and histopathological examination of the resected specimen was also done to confirm the pre-operative diagnosis. All patients underwent wide local resection and reconstruction using custom mega prosthesis performed by our orthopaedic surgical team.
Results: There was no evidence of malignant change in any of our patients. All 8 patients were well with good functional outcome with no evidence of tumour recurrence at the latest follow-up.
Conclusion: Distal humeral GCT is not as uncommon as once thought. The incidence is increasing due to better and prompt health care access and reporting by medical professionals. A high degree of clinical suspicion, good diagnostic techniques and multimodal team approach towards treatment has a positive effect on clinical outcomes for such complex pathologies.
Keywords: Giant cell tumour, Trucut biopsy, Custom mega prosthesis.
Giant cell tumour (GCT) or Osteoclastoma is a common benign tumour affecting the epiphyseal region of a mature skeleton. It commonly manifests in the age group of 25-40 years with a slight female preponderance. The most common site of occurrence of such tumours in decreasing order of frequency are distal femur, proximal tibia and distal radius. However there have been reports in literature of GCT’s presenting in unusual sites such as pelvis, distal humerus and sacrum.[1],[2],[3]In the Indian scenario, the exact number of patients suffering from GCT remains elusive due to the lack of a central monitoring and reporting agency and also due to poor awareness among general population. However in recent times, this has favourably changed with more people having better awareness and better healthcare access. Surprisingly though, the incidence of such tumours in uncommon sites is relatively more than the common sites which still remains high with regard to absolute numbers.
Giant cell tumours are primarily benign which rarely can be either primarily malignant to start with or undergo secondary transformation to malignant chondrosarcoma. Another cause of worry is that since GCT occurs in the epiphyses of long bones, it can involve peri-articular cancellous bone and even invade the articular surface if reporting late to medical centres. The treatment of such tumours involves a multidisciplinary team approach involving pathologists, orthopaedic surgeons, plastic surgeons, medical oncologists, physiotherapists among others. It is absolutely paramount to obtain an accurate pre-operative diagnosis[1] to exclude malignancy and then proceed with a wide local resection (if proven benign) and reconstruct the resected bone with either allograft or metallic endoprosthesis which should provide a stable, mobile and functional elbow.
Since all our patients were from rural background and due to lack of adequate allografts, in our centre we prefer to use modular custom mega prosthesis (CMP) for distal humeral and elbow reconstruction. There have been a few published data of isolated case reports of GCT in unusual sites such as distal humerus.[1][2],[3]In this study we present our small but significant series of eight patients with GCT of distal humerus who underwent operative treatment at our centre.
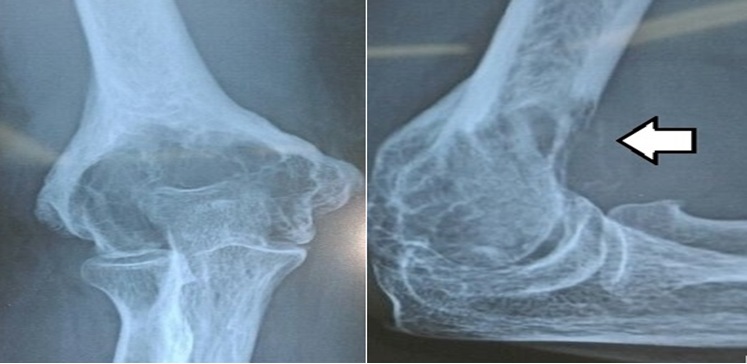
Eight patients (M:F::2:6) (Table.1) presented to us with pain, swelling and difficulty in using the elbow for over 3-6 months. Digital radiographs of the elbow were taken in all which revealed a primary lytic lesion involving distal humerus (Fig. 1). A clinical diagnosis of GCT was confirmed pre-operatively using trucut biopsy. The biopsy specimen was fixed in 10% formalin and then processed further using standard HPE techniques. The disease was classified using the Enneking’s staging system by the orthopaedic surgical team. We specifically looked for any evidence of malignant potential in the biopsy specimen. After excluding malignancy, all 8 patients underwent wide local resection and endoprosthetic reconstruction using CMP by the orthopaedic surgeon.
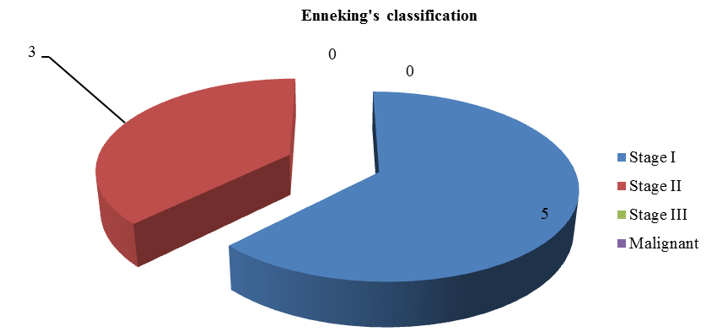
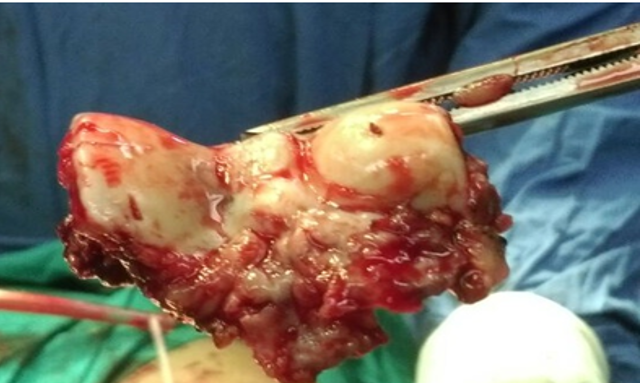
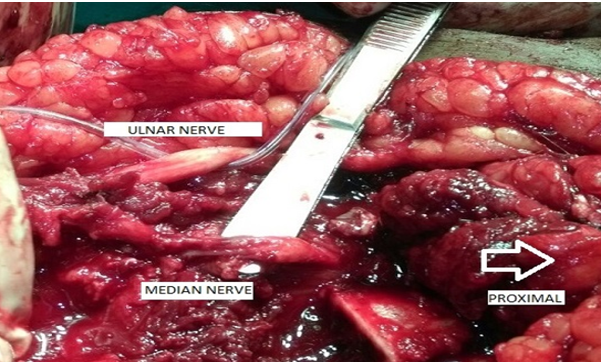
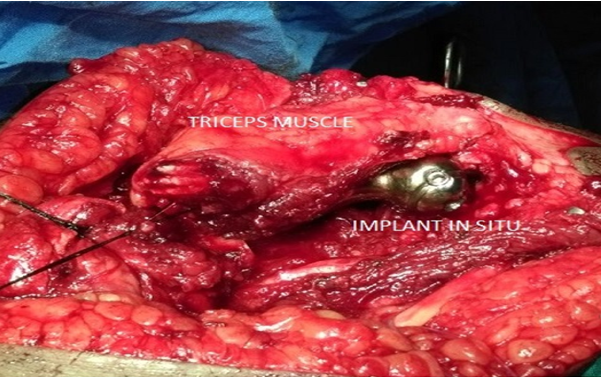
In our series 3 patients had stage II and 5 patients had stage I disease under Enneking staging system (Chart 1). The resection was carried out en bloc if possible but in a majority of our series (7 cases) the bone was resected piece-meal due to the thinned out cortex affected by the disease (Fig. 2). After appropriate preparation of the tumour bed (Fig. 3), humerus and ulna, reconstruction was carried out using a 316 L surgical stainless steel distal humeral CMP (Fig. 4). The soft tissues were repaired over the prosthesis and appropriate wound closure carried out. The resected specimen was subjected to HPE which confirmed our pre-operative diagnosis and also tumour margin clearance. For the bone specimens we used 3-5 mm thick sections which were decalcified using nitric acid solution. Following decalcification, all tissue samples were processed using increasing concentrations of alcohol. Paraffin blocks were prepared and sections taken. The slides were then mounted and viewed under high power microscope.
Post-operatively the patients were placed on an above elbow slab for 3 weeks for soft tissue healing and then started on gentle rehab protocol after input from the orthopaedic surgeon and physiotherapist. The patients were reviewed back at our centre at 6,10,12,18 and 20 weeks and thereafter at 6 monthly intervals. The functional assessment was made using the orthopaedic specific Disabilities of the Arm, Shoulder and Hand (DASH) scoring system.
The average age in our series was 34.33 years. Post-operatively three patients had ulnar nerve neuropraxia due to tension on the nerve intra-operatively which recovered at 12 weeks. At a minimum of one year follow-up all patients were well with good functional outcome with no evidence of tumour recurrence. The average DASH score in our series was 77% with an average of 92° flexion in elbow movement.
Benign bone tumours include a consortium of pathological conditions with varied clinical and radiological presentation.[4] They can either be lytic, sclerotic or mixed[5],[6]depending on the pathology. The differential diagnosis for benign lytic lesions include GCT (skeletally mature) vs Chondroblastoma (skeletally immature), aneurysmal bone cysts or simple bone cysts.[7] GCT by far represents the most common benign bone tumour with a purely lytic component.
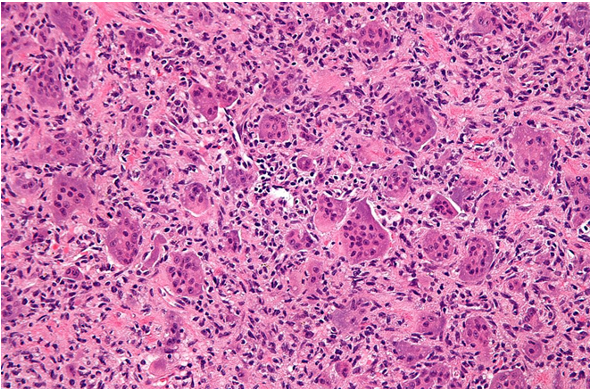
The clinical and microscopic appearance of GCT does not vary between different sites. The classical microscopic appearance has two cell types namely mononuclear stromal cells and osteoclast type giant cells. These osteoclast like giant cells are uniformly distributed throughout the tumour tissue (Fig. 5). Many giant cells are larger than normal osteoclasts with numerous (> 50 nuclei) polygonal chondroblasts with eosinophilic cytoplasm arranged in sheets with no cellular atypia or nuclear pleomorphism. Also another diagnostic indicator is the presence of osteoclast type giant cells.[8]
Novais et al[3] reported a case of multicentric GCT involving predominantly upper limb with lesions of metacarpals, distal radius, phalanges and humerus. He reported recurrence of the metacarpal lesions. In our study we did not report any recurrence which could be explained by the fact that intra-lesional curettage was the preferred treatment adopted by them vs excision in our study. Fernandez et al[9] reported a single case of distal humeral GCT with a DASH score of 80 (excellent outcome) following resection and CMP replacement which is similar to our series (DASH score 77%). Similar results were also reported by Guo et al and other authors.[10],[11],[12]
We believe that the good functional outcome reported in our study is a combination of several key factors namely accurate HPE diagnosis, multidisciplinary approach and excellent post-operative rehab protocols. Distal humerus is now becoming a more frequent site for GCT and the management of such complex tumours should be undertaken in a tertiary care centre with good diagnostic and therapeutic infrastructure. A high index of suspicion along with prompt referral services should improve the overall outcomes of such bone lesions.
Our series does have a few limitations such as relatively short follow-up, smaller case series and more importantly lack of data on long term survivability of such indigenous prosthesis. When compared to more complex, expensive implants our prosthesis might appear basic but with encouraging short to mid term results of such prosthesis, the future does appear promising for these patients who otherwise cannot afford more expensive implants.
Table 1: Master chart with patient demographics
|
S. no. |
Age/Sex |
Diagnosis/ Classification (Enneking’s) |
Follow-up (months) |
Average DASH score |
Outcome |
Remarks |
|
1. |
37/F |
II |
26 |
73 |
Fair |
Ulnar neuroplraxia |
|
2. |
31/F |
II |
33 |
76 |
Good |
|
|
3. |
23/M |
I |
28 |
77 |
Good |
|
|
4. |
34/F |
I |
27 |
71 |
Fair |
Ulnar neuropraxia |
|
5. |
36/M |
II |
24 |
78 |
Good |
- |
|
6. |
45/F |
II |
18 |
78 |
Good |
- |
|
7. |
46/F |
II |
16 |
79 |
Good |
- |
|
8. |
44/F |
I |
12 |
77 |
Good |
Ulnar neuropraxia |
 |
Click here to view |
Chart 1: Patient classification based on Enneking’s staging
 |
Click here to view |
Fig. 1: Pre-op X-ray showing classical lytic lesion involving epiphyseal region of distal humerus. Arrow indicates breach in anterior cortex
 |
Click here to view |
Fig. 2: Resected distal humeral specimen with intact articular surface
 |
Click here to view |
Fig. 3: Clinical picture showing clear tumour bed and neurovascular structures
 |
Click here to view |
Fig. 4: Clinical picture showing after implantation and soft tissue repair
 |
Click here to view |
Fig. 5: Microscopic appearance of giant cell tumour under high power microscope
Giant cell tumour occurring in distal humerus was once a rarity in the past. However recent trends and reports have shown more such cases being reported and managed surgically in tertiary centres. The keystone in successful and prompt treatment still remains an accurate pre-operative diagnosis. Histopathology still remains the gold standard investigation for such common tumours in relatively uncommon sites.
Conflict of Interest: None.
How to cite : Prakasam S, Chitra S, Sulochana, Distal humeral giant cell tumour–Is it still uncommon or just merely underreported. IP J Diagn Pathol Oncol 2019;4(1):45-49
This is an Open Access (OA) journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
Viewed: 2080
PDF Downloaded: 585