- Visibility 312 Views
- Downloads 46 Downloads
- Permissions
- DOI 10.18231/j.jdpo.2021.063
-
CrossMark
- Citation
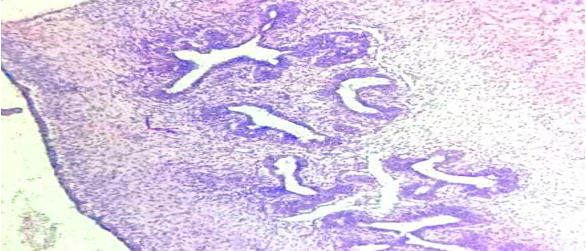
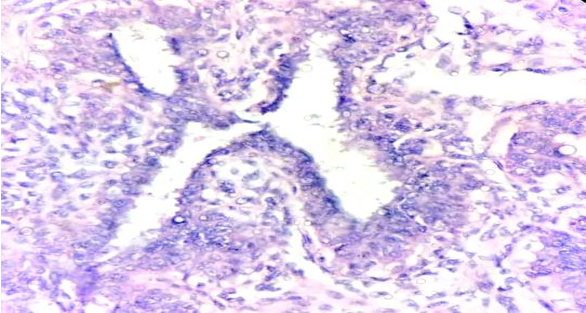
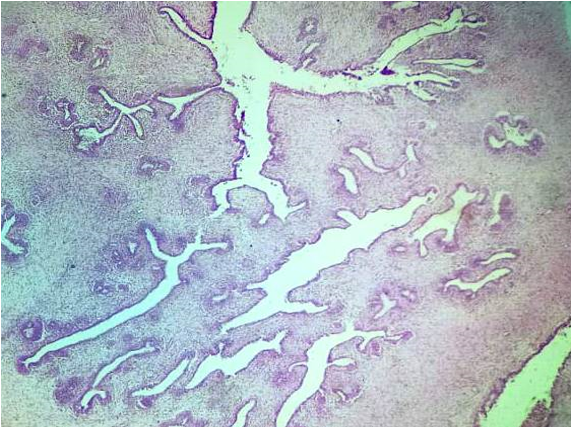
Histopathological study of benign breast lesions
- Author Details:
-
R Poojasree
-
M Anil Kumar
-
A Hareesh Kumar
-
T Nagachandana
-
M Janaki *
Abstract
Introduction: Benign breast lesions are common in young females and are painless. Fibroadenoma is the commonest lesion among all the breast lesions and occurs in any age.
Aims & Objectives: 1: To study the age and sex wise distribution of benign breast lesions; 2: To study the clinicopathological changes of benign breast diseases; 3: To study different types of benign breast lesions; 4. To study the histomorphological changes of benign breast lesions with clinical correlation.
Materials and Methods: A prospective study of two years was done to evaluate the different types, patterns of benign breast lesions in females in relation to age, clinical and radiological features.
Results: A total of 140 benign breast diseases were studied. Fibroadenoma (76; 54.2%) was the most common lesion noted in younger females (18-24yrs) followed by fibrocystic disease (25; 17.8%) & benign phyllodes (14; 10%).
FNAC followed by histopathological examination were the diagnostic criteria used for confirmation of the lesions.
Conclusion: Benign breast lesions were common in young females, presented with painless, mobile breast lumps. Mastalgia and nipple discharge were other symptoms.
Introduction
Benign breast diseases are heterogeneous group of lesions with diverse symptoms and or detected by incidental microscopic findings.[1]
30% of the women suffer from benign breast diseases and require treatment.[2]
The lesions are common in younger population, the incidence rises during the second decade and peak in the fourth and fifth decades. The malignant diseases are more common in the post-menopausal women.[2], [3], [4], [5], [6], [7] These lesions maybe asymptomatic or have visible clinical manifestations such as palpable lump, pain in lump, mastalgia and nipple discharge. These non-specific symptoms are also encountered in various breast diseases, hence further evaluation by imaging techniques (USG & Mammogram) and histopathological study (core biopsy) for definitive diagnosis is mandatory. Love s et al [8] classified (NASHVILLE CLASSIFICATION) benign breast diseases into the non-proliferative lesions, proliferative lesions without atypia, proliferative lesions with atypia. Proliferative breast diseases are proliferation of epithelial cells without atypia are associated with a small increase in the risk of subsequent carcinoma in the breast. [1] These are predictors of risk but are thought to be unlikely precursors of carcinoma. [1], [2], [9], [3], [4], [6], [7], [10], [11] Benign breast diseases are very common but complex process hence requires integrative approach involving the clinician, radiologist and pathologist. [2]
Aims & Objectives
To study the age and sex wise distribution of benign breast lesions
To study the clinicopathological changes of benign breast diseases.
To study different types of benign breast lesions
To study the histomorphological changes of benign breast lesions with clinical correlation.
Materials and Methods
The prospective study was conducted in the Department Of Pathology, Santhiram Medical College and Hospital, Nandyal, Kurnool for a period of 2 years, i.e from December 2018 to November 2020. All the female patients of the breast disease irrespective of the age admitted/ attended in the Santhiram Hospital from in and around Nandyal were selected for the study. Relevant clinical data obtained from the hospital records.
Institutional ethical committee clearance was taken for the study. A total of 140 female patients with clinical and radiological diagnosis of benign breast diseases were included in the study.
Inclusion criteria
Female patients irrespective of age, presenting with breast lumps, pain, mastalgia and nipple discharge were included in the study.
Patients with clinical, radiological, cytological and histopathological data were included.
Exclusion criteria
Women with malignant diseases.
Patients on radiotherapy and chemotherapy.
Lactating women and women with breast abscess were excluded from the study.
After the clinical diagnosis, the patients were subjected for radiological investigations likes USG, Mammogram & MRI.
FNAC followed by Tru-Cut biopsy and excision biopsy. The excised tissue was fixed in 10% Formalin & routine processing was done. The H&E stained sections examined under light microscope. Histopathological diagnosis was correlated with clinical, radiological and cytological findings.
Results
In the present study, 140 cases were evaluated.
Majority of Benign breast diseases were highest in the age group of 21-30 years (86 cases, 61.4%). Least common affected in the age group of below 20yrs (2 cases, 1.4%) and more than 50 years (1 cases, 0.7%).
The most common presentation was lump in the breast (116 cases, 82.7%), Painless lump (90 cases 64.2%), with Pain (26 cases,18.5%), nodularity (14cases, 10%) and nipple discharge (10 cases, 7.1%) were the other presenting complaints. More than one symptom was present in the same patient. Pain in both breast was noted in more than 50 cases. The pain was cyclical in 20 cases and non-cyclical in 10 cases. Only one case (1.3%) presented with nipple discharge with palpable lump & pain in breast.
Site
The and right breast in 74cases (52.8%) patients and the left breast affected in 60 cases (42.2%) patients. In 6cases (4.2%) patients both the breasts were affected. Majority of the breast lumps were located in upper outer quadrant 100 cases (71.4%), followed by lower inner quadrant 30 cases (21.4%) and least in upper inner quadrant 10 cases (7.1%).
Size
Minimum size of the breast lump was 1-2 cms and maximum size being 10cms. Majority of the breast lump were with the size range from 3-5cms (50cases; 35.6.8%) followed by 2-3cms (40cases; 28.5%). Fibroadenoma in the size range of 2-3cm [40 cases 28.5%]. More than 5cms size was mostly noted in phyllodes tumour and proliferative breast disease with and without atypia lesions (22 cases; 15.7%) Fibroadenoma (76; 54.2%) was the most common lesion followed by Fibroadenosis (25; 17.8%), proliferative breast disease with atypia (8; 5.7%), without atypia (16; 11.4%) and benign phyllodes tumour (14; 10%).
|
Clinical features |
Number |
% |
|
Breast Lump Painless |
90 |
64.2% |
|
Breast Lump Asco Pain |
26 |
18.5% |
|
Nipple Discharge] |
10 |
7.1% |
|
Nodularity |
14 |
10% |
|
Location |
Number |
% |
|
Upper Inner Quadrant |
10 |
7.1% |
|
Upper Outer Quadrant |
100 |
71.4 % |
|
Lower Inner Quadrant |
30 |
21.4% |
|
Size |
Number |
% |
|
1 – 2 cms |
28 |
20% |
|
2 – 3 cms |
40 |
28.5% |
|
3 - 4 cms |
25 |
17.8% |
|
4 - 5 cms |
25 |
17.8% |
|
5 & > 5 cms |
22 |
15.7% |
|
Lesion |
Right |
Left |
Bilateral |
|
Fibroadenoma |
46(32.8%) |
30(21.4%) |
- |
|
Fibroadenosis |
10(7.1%) |
12(8.5%) |
3(2.1%) |
|
Intraductal Papilloma |
- |
1(0.7%) |
- |
|
Benign Phyllodes Tumour |
4(2.8%) |
7(5%) |
3(2.1%) |
|
Proliferative Breast Disease Without Atypia |
10(7.1%) |
6(4.2%) |
- |
|
Proliferative Breast Disease With Atypia |
4(2.8%) |
4(2.8%) |
- |
|
Total |
74 |
60 |
6 |
|
% |
52.8% |
42.2% |
4.2% |
|
Lesion |
10-20 yrs. |
20-30 yrs. |
30-40 yrs. |
40-50 yrs. |
50-60 yrs. |
Total |
% |
|
Fibroadenoma |
2 |
52 |
20 |
2 |
- |
76 |
54.2% |
|
Fibroadenosis |
- |
14 |
8 |
2 |
1 |
25 |
17.8% |
|
Intraductal Papilloma |
- |
- |
1 |
- |
- |
1 |
0.7% |
|
Benign Phyllodes Tumour |
- |
8 |
6 |
- |
- |
14 |
10% |
|
Proliferative Breast Disease Without Atypia |
- |
10 |
4 |
2 |
- |
16 |
11.4% |
|
Proliferative Breast Disease With Atypia |
- |
2 |
4 |
2 |
- |
8 |
8% |
|
Total |
2 |
86 |
43 |
8 |
1 |
140 |
100% |
|
% |
1.4% |
61.4% |
30.7% |
5.7% |
0.7% |
|
|
Discussion
Physiological changes in the breast are hormonal dependant. They are maturation, cyclical & reproductive changes and involution of breast. The exaggerated physiological changes results as a disorder.[12] The presentation of benign breast disorders are variable as breast lump; lump with or without pain, nodule, axillary swelling, unilateral or bilateral breast pain, nipple discharge.
In this study the common presenting symptom was breast lump 116 cases (82.8%). Foncroft LM et al 2001 (87.4%), [13] Ratana chaikamont T et al 2005 [14] (72.3%), Sangma et al 2013 [15] (87%) documented that the breast lump was the most the commonest presentation, Our study correlated with the above authors.
And dint correlate with Trupti P Tonape et al 2018(58%)[12] Satyajit Samal 2019 et al (53%), [2] Ilaiah M et al 2015[16] (58.3%), Chalya PL et al 2016[17] (67.6%)
Mastalgia (26cases; 18.5%) and nodularity (14 cases; 10%) was noted in 26+14=40 cases (28.5%). 30% by Koorapati Ramesh et al 2017 [1] and 27.7% of cases by Satyajit Samal et al 2019.[2] Hence our study correlated.
The incidence of mastalgia was 26cases (18.5%) in the present study was equal with Sangma et al 2013 [15] who reported 33% cases., 12.8% to 30.3% range by La Vecchia C et al 1985. [7]
The incidence of nipple discharge was 9% La Vecchia C et al 1985,[18] 8% by Sangma et al 2013, 8% by Koorapati Ramesh et al 2017. [1] Our study showed 14 cases (10%) and correlated with the above authors.
In the present study 52.8% (74/140) cases had right breast lesion, 42.8% (60/140) had left breast and 6 cases (4.2%) had both breast lesions. Koorapati Ramesh et al 2017. [1] had 52%, 32% and 16%. Chalya PL et al 2016 [17] had 53.8%, 42.8% and 3.4%,. Sangma et al 2013 [15] 48%, 40%, 12% and Shambhu Kumar Singh et al 2016 [19] 54.8%, 45.16% Our study correlated with the above author’s study.
Trupti P Tonape et al 2018[12] reported 44% (50 cases) in left breast and 40% in right breast. 42.8% (60/140 cases) in the present study and differed with Trupti P Tonape et al 2018. [12]
Sangma et al 2013[15] and Koorapati Ramesh et al 2017 [1] reported 12% & 16% cases with bilateral breast involvement respectively. The present study showed (4.2%) 6/140, hence differed with above author’s studies.
Majority of the breast lumps 100 cases (71.4%), were located in upper outer quadrant followed by lower inner quadrant 30 cases (21.4%) and least in upper inner quadrant 10 cases (7.1%). Our study correlated with Koorapati Ramesh et al 2017.[1] [60%,8%], Chalya PL et al 2016[17] [63.8%, 6.8%]. Trupti P Tonape et al 2018[12] documented that upper inner quadrant (30%) followed by upper outer quadrant (24%). Our study differed with Trupti P Tonape et al 2018.[12]
In the present study, the commonest age group was 20-30 years (86; 61.4%), and second common age group being 30-40 years (43; 30.7%) correlated with, Koorapati Ramesh 2017.[1] (60%), Ilaiah M et al 2015[16] (58.3%) Trupti P Tonape et al 2018 [12] (26%) Satyajit Samal et al 2019[2] (22%) & S David Nathanson et al 2014.[20]
In the present study, the youngest patient was 16 years of age, the oldest being 50 years. Similar observation made by Satyajit Samal et al 2019[2] and Koorapati Ramesh et al 2017.[1] In the present study, least commonly affected age group was above age 50 years (1 case 0.7%).Our study correlated Trupti P Tonape et al 2018[12] (2%) differed with Koorapati Ramesh et al 2017[1] (4%) and Sangma et al 2013[15] (4%).
In the present study, fibroadenoma was the most common benign breast lesion (76/140 cases 54.2%) (in the age range of 20-30 years). Similar observation made by Navneet Kaur et al 2012.[21] Koorapati Ramesh et al 2017 [1] Observed 56.8% (142/250). Our study corelated with Sangma et al 2013 [16] (48%), Koorapati Ramesh et al 2017.[1] (56.8%), Trupti P Tonape et al 2018[12] (42%),46.6 & 55.6% by Adesunkami AR et al 2001,[22] Ihekwaba FN et al 1994[23] and Greenberg R et al 1998. [24]
The second common lesion was Fibroadenosis in 3rd and 4th decade 25/140 cases(17.8%).Similar observations made by Ihekwaba FN et al 1994[23] (19.7%), Sangma et al 2013[16] (18%) Florica JV et al 1994.[25] Our study correlates with the above authors study.
Dupont WD et al 1985[26] identified proliferative breast diseases with atypia as 4.%, 4.6% by Sangma et al 2013.[16] In the present study 8 cases; 5.7% observed, our study correlated with the above authors study and differed with Chalya PL et al 2016 [17] (2%). There is 4 fold increase risk in proliferative breast diseases with atypia.[16] Currently there is controversy over the classification of proliferative breast lesions and the microscopic risk assessment, causing less relevance in clinical practice.[16] Hence there is need for new-morphological marker-genetic and molecular.
Conclusion
Benign breast disease is a common problem in women among 21-30 years. The common clinical presentations is painless mobile breast lump. Care should be taken to differentiate it as benign and or with malignant differentiation through clinical, radiological and histopathological assessment. There is no consensus on morphological risk factors, hence there is need for molecular and genetic study, which help in early detection of risk of malignancy and better clinical management.
Conflict of Interest
The authors declare that there are no conflicts of interest in this paper.
Source of Funding
None.
References
- Ramesh K, Bookya K. A study on clinical and pathological correlation of benign breast lesions. Int Surg J. 2017;4(8):2700-5. [Google Scholar] [Crossref]
- Samal S, Swain P, Pattnayak S. Clinical, pathological and radiological correlative study of benign breast diseases in a tertiary care hospital. Int Surg J. 2019;6(7):2428-32. [Google Scholar] [Crossref]
- Kelsey JL, Gammon MD. The epidemiology of breast cancer. CA Cancer J Clin. 1991;41(3):146-65. [Google Scholar] [Crossref]
- Fitzgibbons PL, Henson DE, Hutter RV. Benign breast changes and the risk for subsequent breast cancer: an update of the 1985 consensus statement. Cancer Committee of the College of American Pathologists. Arch Pathol Lab Med. 1998;122(12):1053-5. [Google Scholar]
- Sarnelli R, Squartini F. Fibrocystic condition and at risk, lesions in asymptomatic breasts: a morphologic study of postmenopausal women. Clin Exp Obstet Gynecol. 1991;18(4):271-9. [Google Scholar]
- Cook MG, Rohan TE. The Patho-epidemiology of benign proliferative epithelial disorders of the female breast. Pathol. 1985;146(1):1-15. [Google Scholar] [Crossref]
- Vecchia CL, Parazzini F, Franceschi S, Decarli A, . Risk factors for benign breast disease and their relation with breast cancer risk. Pooled information from epidemiologic studies. Tumori. 1985;71(2):167-78. [Google Scholar]
- Love SM, Gelman RS, Silen W. Sounding board. Fibrocystic "disease" of the breast--a nondisease?. N Eng J Med. 1982;309(16):1010-4. [Google Scholar] [Crossref]
- Caleffi M, Filho DD, Graudenz MBK, Littrup PJ, Freeman-Gibb LA. Cryoablation of benign breast tumours: evolution of technique and technology. Breast. 2004;13(5):397-407. [Google Scholar] [Crossref]
- Kumar V, Abbas A, Aster J. Robbins & Cotran Pathologic Basis of Disease. 9th Edition. 2018;2. [Google Scholar]
- Hughes L, Mansel R, Webster DT. Aberrations of normal development and involution (ANDI): a new perspective on pathogenesis and nomenclature of benign breast disorders. Lancet. 1987;5(8571):1316-9. [Google Scholar]
- Tonape T, Tulsian A, Gope D, Jyotsna C. A study of clinical patterns in benign breast disorders. Int Surg J. 2018;5(2). [Google Scholar] [Crossref]
- Foncroft LM, Evans EB, Hirst C, Hicks BJ. Presentation and diagnosis of adolescent breast disease. Breast. 2001;10(5):399-404. [Google Scholar]
- Ratana T. Clinical breast examination, palpable breast lesion. J Med Assoc Thai. 2005;88(4):505-7. [Google Scholar]
- Sangma MB, Panda K, Dasiah S. A clinico-pathological study on benign breast diseases. J Clin Diagn Res. 2013;7(3):503-6. [Google Scholar]
- Ilaiah M, Purnaiah M, Pasha M. Evaluation of Benign Breast Diseases with Clinico, Pathological and Radiological Correlation. Indian J Appl Res. 2015;5(11). [Google Scholar]
- Chalya PL, Manyama M, Rambau PF, Kapesa A, Ngallaba SE, Masalu N. Clinicopathological pattern of benign breast diseases among female patients at a tertiary health institution in Tanzania. Tanzania J Health Res. 2016;18(1). [Google Scholar] [Crossref]
- Rosai J. Ackermann’s Textbook of surgical pathology. 11the Edn.. 2018;1. [Google Scholar]
- Singh S, Pankaj D, Kumar R, Mustafa R. A clinico-pathological study of malignant breast lump in a tertiary care hospital in Kosi region of Bihar, India. Int Surg J. 2016;3(1):32-6. [Google Scholar] [Crossref]
- Shas R, Rosso K, Nathanson SD. Pathogenesis, prevention, diagnosis and treatment of breast cancer. World J Clin Oncol. 2014;5(3):283-98. [Google Scholar] [Crossref]
- Kaur N, Agarwal N, Panwar P, Mishra K. Clinicopathologic profile of benign breast conditions in Indian women: prospective study based on aberrations of normal development and involution classification. World J Surg. 2012;36(9):2252-8. [Google Scholar] [Crossref]
- Adesunkami AR, Agbakwuru EA. Benign breast disease at Wesley Guild Hospital, Ilesha, Nigeria. West Afr J Med. 2001;20(2):146-51. [Google Scholar]
- Ihekwaba FN. Benign breast disease in Nigerian women: a study of 657 patients. J R Col Surg Edin. 1994;39(5):280-3. [Google Scholar]
- Greenberg R, Skornick Y, Kaplan O. Management of breast fibroadenomas. J Gen Inter Med. 1998;13(9):640-5. [Google Scholar] [Crossref]
- Fiorica JV. Fibrocystic changes. Obstet Gynecol Clin North Am. 1994;21(3):445-52. [Google Scholar]
- Dupont WD, Page DL. Risk factors for breast cancer in women with proliferative breast disease. N Engl J Med. 1985;312(3):146-51. [Google Scholar] [Crossref]
How to Cite This Article
Vancouver
Poojasree R, Kumar MA, Kumar AH, Nagachandana T, Janaki M. Histopathological study of benign breast lesions [Internet]. IP J Diagn Pathol Oncol. 2021 [cited 2025 Oct 01];6(4):295-300. Available from: https://doi.org/10.18231/j.jdpo.2021.063
APA
Poojasree, R., Kumar, M. A., Kumar, A. H., Nagachandana, T., Janaki, M. (2021). Histopathological study of benign breast lesions. IP J Diagn Pathol Oncol, 6(4), 295-300. https://doi.org/10.18231/j.jdpo.2021.063
MLA
Poojasree, R, Kumar, M Anil, Kumar, A Hareesh, Nagachandana, T, Janaki, M. "Histopathological study of benign breast lesions." IP J Diagn Pathol Oncol, vol. 6, no. 4, 2021, pp. 295-300. https://doi.org/10.18231/j.jdpo.2021.063
Chicago
Poojasree, R., Kumar, M. A., Kumar, A. H., Nagachandana, T., Janaki, M.. "Histopathological study of benign breast lesions." IP J Diagn Pathol Oncol 6, no. 4 (2021): 295-300. https://doi.org/10.18231/j.jdpo.2021.063
