- Visibility 74 Views
- Downloads 10 Downloads
- DOI 10.18231/j.jdpo.2020.072
-
CrossMark
- Citation
Profile of fungal opportunistic infection in HIV/ AIDS patients: An appraisal at Indian tertiary care
- Author Details:
-
Ravikanti
-
Rajeshwari K *
-
Sunitha B R
-
G Vishwanath
Introduction
AIDS is an emerging pandemic viral infectious disease caused by Human Immunodeficiency Virus, which has posed the greatest challenge to public health in modern world. Clinical manifestations in HIV infections are primarily due to viral cytopathology and are secondary to the failure of both cellular and humoral immune response.[1], [2], [3], [4], [5]
Opportunistic infections with low CD4 counts influence the morbidity and mortality due to HIV infections. [1], [3], [5], [6] Patients with CD4 counts >200 /mm3 are 6 times more likely to develop opportunistic infections compared to those with CD4 counts of > 350/mm.3
In India, Tuberculosis is the most commonly reported opportunistic infection with CD4 cells >200 / mm3. [2], [3] Other commonly reported opportunistic infections among HIV infected are Oral Candidiasis, Herpes zoster, Cryptococcal Meningitis, Cerebral Toxoplasmosis and Cytomegalovirus Retinitis with CD4 counts < 200 /mm3. [6], [7]
The high incidence of commonly reported opportunistic infections with low CD4 counts in Indian HIV infected individuals highlights the need for early screening and also the need to increase awareness in health care providers in order to improve decisions regarding prophylaxis for prevention and appropriate therapeutic interventions. [7], [8], [9]
To determine role of CD4 decline and the incidence of opportunistic infections, CD4 counts as a clinical score serve as both an alarm for timing of prophylaxis and a guide for therapeutic intervention. [2], [3], [6], [10]
It is also documented that types of opportunistic infections is profoundly influenced by geography and prevalence of infectious diseases in particular region, nutritional, socioeconomic conditions and other factors. [1], [2], [11], [7] Therefore this study will be conducted to evaluate the correlation between CD4 counts in HIV infected patients with onset of specific opportunistic infections. [1], [2], [7], [9]
Materials and Methods
Source of data
This was a prospective study involving proven Fungal cases of HIV/AIDS with signs and symptoms of opportunistic infections attending the outpatient department or admitted to Hospitals during the one year period, from June 2017 to June 2018 from the study group.
Sample size
500 HIV/AIDS seropositive patients with signs and symptoms of OIs, clinically, radiologically and diagnostically proven cases. Informed consent was taken from all patients during the study.
Method of collection of data
Inclusion criteria
Confirmed HIV seropositive cases seeking medical care for signs and symptoms of opportunistic infections like PUO, Fungal infections, Candidiasis, Cryptococcosis, Pneumocystosis, Histoplasmosis, Coccidiodosis. Pneumocystis carinii, Lymphadenopathy, Refractory anemia, Idiopathic Thrombocytopenia.
Exclusion criteria
HIV seropositive individuals already on antiretroviral therapy, asymptomatic partners and children of HIV seropositive individuals, HIV seropositive individuals detected during routine ANC checkup, pre-operative, pre-employment and pre-insurance screening.
Methods of specimen collection
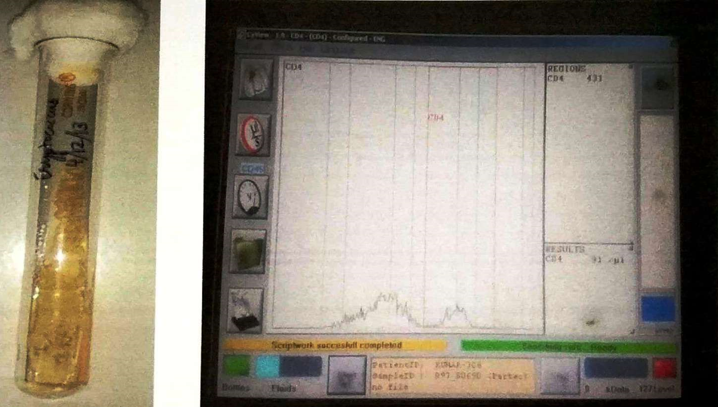
Specimen for CD4 count
With strict aseptic precautions, 3ml of venous blood sample was collected by venepuncture using EDTA vacutainer and processed by flow cytometry, according to the standard protocol supplied by the manufacturer. (PARTEC IVD FLOW CYTOMETER machine, by Partec Gmbh. Am Flugplatg 13. D-02828 Gorlitz. Germany).
Principle
The mouse monoclonal antibody MFM-241 recognizes the human CD4 antigen, a transmembrane glycoprotein (55 kDa) of the immunoglobulin supergene family, present on a subset of T-lymphocytes ("helper/inducer" T-cells) and also expressed at a lower level on monocytes, tissue macrophages and granulocytes. Approximately 20-60% of human peripheral blood mononuclear cells as well as a subpopula-tion of monocytes but with a weaker signal are stained The antibody has been studied at the 8th International Workshop on Human Cell Differentiation Molecules HCDM (former HLDA VIII), May 2006, Quebec, Canada. CD4 is the primary cellular receptor for the human immunodeficiency virus (HIV).
Flow cytometric analysis
CD4-PE fluorescence can be analysed on a Partec Flow Cytometer with an excitation light source of 488 nm or 532 nm (blue or green solid state laser). To count CD4+ T-cells transfer the test tube with 84ftul of the ready prepared blood sample (see Method) to the Partec counting results will be displayed automatically as CD4+ T-cells per µl whole blood.
Method
20 µl whole blood (EDTA as anticoagulant) were taken in a Partec test tube.
20 µl of CD4 mAb PE then added and mixed gently, later incubated for 15 minutes at room temperature protected from light.
800 µl of no lyse buffer is added to Partec test tube and shaken or vortexed gently.
Blood samples were then analyzed on a Partec device by aspiration and results displayed on screen were noted.
All clinical, radiological and laboratory data available,which includes baseline investigations in all HIV seropositive individuals, screening and confirmation for HIV infections available [Strategy III WHO] were recorded & documented in standard proforma for later analysis.
Statistical analysis
The collected data was tabulated, analyzed and subjected for statistical analysis using SPSS 19.0. Results are presented as range for quantitative data and number and percentage for qualitative data.
Results
The present study was carried out on 500 HIV seropositive patients with signs and symptoms of 65 Fungal opportunistic infections attending District Hospital, ART center, over a period of 12 months (June 2017 to May 2018), to know the incidence of fungal infections and their correlation with CD4 count.
The observations made from the study are shown in the following
|
Age |
No. of cases |
Percentage |
|
<20 |
35 |
7.0 |
|
21-30 |
76 |
15.2 |
|
31-40 |
189 |
37.8 |
|
41-50 |
143 |
28.6 |
|
51-60 |
39 |
7.8 |
|
>60 |
18 |
3.6 |
|
Total |
500 |
100.0 |
In our study out of 500 cases includes age group of < 20yrs to > 60yrs, maximum cases noted were 189(37.8%) cases with age group of 31-40yrs,18 (3.6%) cases were least group with age group > 60yrs.
|
Sex |
No. of cases |
Percentage |
|
Male |
276 |
55.2 |
|
Female |
224 |
44.8 |
|
Total |
500 |
100.0 |
Among gender distribution of cases, maximum cases were 276 (55.2%) noted in males, with a male: female ratio of 1.2:1.
|
Risk Factor |
No. of Cases |
Percentage |
|
Heterosexual |
434 |
86.8 |
|
Msm |
9 |
1.8 |
|
Injecting Drug Use |
2 |
0.4 |
|
Blood Transfusion |
12 |
2.4 |
|
Mother To Child |
22 |
4.4 |
|
Probable Unsafe Injection |
9 |
1.8 |
|
Commercial Sex Work |
9 |
1.8 |
|
Truck Driver |
3 |
0.6 |
|
Total |
500 |
100.0 |
In our study, we found majority of study group were 434 (86.8%) cases belongs to heterosexual risk group, least study group 2(0.4%) cases belongs to injecting drug use.
|
Who Grading |
No. of cases |
Percentage |
|
1 |
6 |
1.2 |
|
2 |
95 |
19.0 |
|
3 |
277 |
55.4 |
|
4 |
122 |
24.4 |
|
Total |
500 |
100.0 |
According to WHO Grading, out of 500 cases, majority were belongs to Grade 3, accounting for 277 (55.4%) of the cases.
|
Occupation |
No. o f cases |
Percentage |
|
Agricultural Labourer |
157 |
31.4 |
|
Non Agricultural Labourer |
102 |
20.4 |
|
Domestic Servant |
3 |
0.6 |
|
Skilled Worker |
14 |
2.8 |
|
Semi Skilled Worker |
4 |
0.8 |
|
Petty Buisiness/Small Shop/Self Employed |
28 |
5.6 |
|
Service(Govt/Pvt) |
20 |
4.0 |
|
Student |
20 |
4.0 |
|
Truck Driver/Helper |
10 |
2.0 |
|
Local Transport Worker |
19 |
3.8 |
|
Hotel Staff |
7 |
1.4 |
|
Agricultural Cultivator/Land Holder |
11 |
2.2 |
|
Unemployed |
11 |
2.2 |
|
Retired |
10 |
2.0 |
|
House Wife |
84 |
16.8 |
|
Total |
500 |
100.0 |
We observed that occupation wise distribution of cases maximum cases belongs to agricultural labourer accounting for 31.4% of the cases,
|
Diseases |
No.of Cases |
Mean Cd4 Count |
|
Oral Candidiasis |
46(9.2.%) |
156 |
|
Pnuemocystitis Zeroveci |
4(0.8%) |
240.9 |
|
Vaginal Candidiasis |
5(1%) |
258.5 |
|
Oesophageal Candidiasis |
5(1%) |
144.9 |
|
Cryptococcal Meningitis |
2(0.4%) |
55 |
|
Aspergillus otomycosis |
3(0.6%0 |
170 |
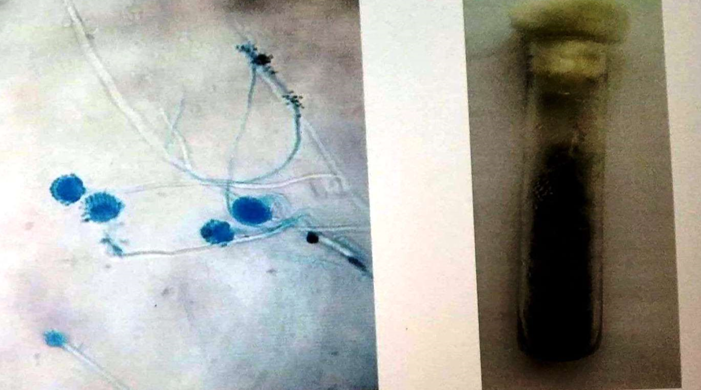
In our study we noted 65(13%) cases of fungal infections with majority of cases with oral candidiasis.
There was a statistically significant association between age, risk factor and WHO Grading and CD 4 count and “P” value less than 0.05. There was no statistically significant association between gender, occupation and CD 4 count.



Discussion
In the present study the clinical profile of various fungal opportunistic infections among HIV seropositive patients admitted were analyzed.
Maximum numbers of HIV positive individuals (37.8%) were in the age group of 31-40 years. Several study groups both in India and abroad have reported 48.2% to 92% HIV seropositive individuals in this age group. Our findings are in accordance with Vajpayee et al.
|
Authors |
Age group (%) |
|
Vajpayee et al 2003 [8] |
48.2% |
|
A. Singh et al 2003 [9] |
92% |
|
A. Wadhwa et al 2007 [12] |
82% |
|
Saldanha et al 2008 [13] |
74.8% |
|
Present study |
43.8% |
Male: female ratio in the present study was 1.2:1. Our findings are in consistent with Vickers et al study showed 1.4:1. While the males belonged to a wide age spectrum, the females were a considerably younger population, and most of them acquired infection from their spouses, reflecting the male dominance in Indian society and emphasizing an increased need for awareness and counseling of both spouse.
|
Authors |
CD4 count (%) |
|
Sharma et al 2004 [14] |
82.5% |
|
A. Wadhwa et al 2012 [12] |
60% |
|
Anantha A. et al 2012 [15] |
46.2% |
|
Ghate et al 2009 [11] |
69.6% |
|
Michael O. Iroezindu et al 2013 [16] |
95% |
|
present study |
64% |
|
Authors |
Candida |
Cryptococcus |
Aspergillus |
Pencilium |
Pneumocystic jeroveci |
|
Ghate et al 2000 [11] |
11.6% |
- |
- |
- |
7% |
|
Sing et al 2003 [9] |
59% |
47% |
- |
- |
6% |
|
Kumarsamy et al 2005 [17] |
70% |
- |
- |
- |
- |
|
Chakravarthy et al 2006 [10] |
20.3% |
1.4% |
- |
- |
- |
|
Saldnaha et al 2008 [13] |
34.5% |
- |
- |
- |
- |
|
Ghate et al 2009 [11] |
11.3% |
1.7% |
- |
- |
- |
|
Madkar et al 2012 [16] |
37.6% |
- |
- |
- |
- |
|
Pradeep et al 2013 [18] |
22% |
- |
- |
- |
- |
|
Present study |
11.2% |
0.4% |
0.3% |
0.3% |
- |
Our findings are consistent with Ghate et al study. [11] The lower CD4 counts in present study may be due to a diagnostic bias from later detection of the disease reflecting a paucity of extensive diagnostic facilities at the peripheral health care centers, so that the diagnosis remains uncertain or is not established until late stages, when significant immunosuppression has already set in and patients are referred to tertiary health care centers. [1], [13]
The findings of low CD4 counts at admission to the hospital demonstrate that a high level of immunodeficiency was already present, defining advanced AIDS.
Epidemiological features depend upon social and cultural practices of the people which may again vary from region to region.
Our findings are in accordance with Ghate et al [11] study. Oral candidiasis was the commonest mucocutaneous opportunistic infection observed in our study. The number of T-helper cell usually fall over the course of HIV infection. Serious fungal infections tend to occur, when T-helper cell count has dropped to around 100 mm3.
Cryptococcal meningitis is the most common type of meningitis reported in important neurological studies in India. Cryptococcal meningitis, an AIDS – defining illness, usually appears when CD4 counts are below 100/mm3 and is associated with an increased risk of death.
Four of the HIV seropositive patients were co-infected with pneumocystis carinii pneumonia (PCP) in the present study. It is now established that PCP is one of the common opportunistic infections in HIV but the cases are relatively less documented, may be due to the lack of routine testing facility. PCP is rarely documented in India
Our study correlates with Ghate et al [11] and Vajapyee et al [8] with CD4 count <100.
Four percent of the HIV seropositive patient had polymicrobial infections, which included oral candidiasis plus pulmonary tuberculosis in 2% and PCP plus cryptosporidial infestation in 2%.
About one percent of HIV seropositive cases of present study were co-infected with Hepatitis B virus. All the co-infected patients were under gone blood transfusion previously.
Conclusions
HIV/AIDS is the burning crisis worldwide. Early diagnosis of opportunistic infections and prompt treatment improves the quality of life, increases the life expectancy among infected patients and delays progression to AIDS. Timely initiation and continuous intake of ART will not only prolong the survival but will also decrease the viral load a transmission of the disease.
Source of Funding
No financial support was received for the work within this manuscript.
Conflict of Interest
The authors declare they have no conflict of interest.
References
- T R Sterling, R E Chaisson, Mandell GL, Bennett JE, Dolin R. General clinical manifestation of HIV infections (including retroviral syndrome and oral, cutaneous, renal, ocular, metabolic and cardiac disease). Principles and practice of infectious diseases 2010. [Google Scholar]
- A S Fauci, H Chiffordlane, D L Lango, D L Kasper, J L Jameson, A S Fauci. Human immunodeficiency virus disease, AIDS and related disorders. Harrison’s principles of internal medicine 2008. [Google Scholar]
- M Ghate, S Deshpande, S Tripathy, M Nene, P Gedam, S Godbole. Incidence of common opportunistic infections in HIV-infected individuals in Pune, India: analysis by stages of immunosuppression represented by CD4 counts. Int J Infect Dis 2005. [Google Scholar]
- C B Holmes, R Wood, M Badri, S Zilber, B Wang, G Maartens. CD4 Decline and Incidence of Opportunistic Infections in Cape Town, South Africa. J Acquir Immune Defic Syndr 2006. [Google Scholar] [Crossref]
- Brambillia, B Nocita, H Hasson, E Boeri, F Veglia, A Castagna. Relation Between CD4 Cell Counts and HIV RNA Levels at Onset of Opportunistic Infections. J Acquir Immune Defic Syndr 2001. [Google Scholar]
- P Pongsai, K Atamasirikul, S Sungkanuparph. The role of serum cryptococcal antigen screening for the early diagnosis of cryptococcosis in HIV-infected patients with different ranges of CD4 cell counts. J Infect 2010. [Google Scholar] [Crossref]
- A S Fauci, HC Lane, Hauser, Longo, Jameson, Kasper, Braunwald, Fauci. HIV disease: AIDS and related disorders. Harrison’s Principles of Internal Medicine 2005. [Google Scholar]
- M. Vajpayee, S. Kanswal, P. Seth, N. Wig. Spectrum of Opportunistic Infectionsand Profile of CD4+ Counts among AIDSPatients in North India. Infect 2003. [Google Scholar] [Crossref]
- A Singh, I Bairy, P G Shivananda. Spectrum of opportunistic infections in AIDS cases. Indian J Med Sci 2003. [Google Scholar]
- J Chakravarty, H Mehta, A Parekh, S V S Attili, N R Agarwal, S P Singh. Study on clinic-epidemiological profile of HIV patients in Eastern India. J Assoc Physicians India 2006. [Google Scholar]
- M Ghate, S Deshpande, S Tripathy, M Nene, P Gedam, S Godbole. Incidence of common opportunistic infections in HIV-infected individuals in Pune, India: analysis by stages of immunosuppression represented by CD4 counts. Int J Infect Dis 2009. [Google Scholar] [Crossref]
- A Wadhwa, R Kaur, S K Agarwal, S Jain, P Bhalla. AIDS-related opportunistic mycoses seen in a tertiary care hospital in North India. J Med Microbiol 2007. [Google Scholar] [Crossref]
- D Saldanha, N Gupta, S Shenoy, V Saralaya. Prevalence of opportunistic infections in AIDS patients in Mangalore, Karnataka. Trop Doctor 2008. [Google Scholar] [Crossref]
- S S Madkar, A J Vankudre, S L Nilekar. Spectrum of opportunistic infections in HIV-AIDS patients. Indian J Comm Health 2012. [Google Scholar]
- A A Takalkar, G S Saiprasad, V S Prasad, N S Madhekar. Study of opportunistic infections in HIV seropositive patients admitted to community care centre (CCC), KIMS Narketpally. Biom Res 2012. [Google Scholar]
- M O Iroezindu. Prevalence and Risk Factors for Opportunistic Infections in HIV Patients Receiving Antiretroviral Therapy in a Resource-Limited Setting in Nigeria. J AIDS Clin Res 2013. [Google Scholar] [Crossref]
- P Bhaumik, K Debnath, B Sinha. Spectrum of opportunistic infections among HIV/AIDS patients of Tripura. JIACM 2013. [Google Scholar]
- N Kumarasamy, S Vallabhaneni, T P Flanigan, K H Mayer, S Solomon. Clinical profile of HIV in India. Indian J Med Res 2005. [Google Scholar]
